MIRECC / CoE
Toolkit for Providers of Clients with Co-occurring TBI and Mental Health Symptoms

Why an On-line Toolkit?
 Traumatic Brain Injury (TBI) is a significant public health concern. This toolkit provides mental health clinicians necessary information to address the needs of Veterans/Military Personnel with a history of TBI and co-occurring mental health conditions. Community mental health clinicians’ input was integral in identifying areas of focus. This toolkit is designed to assist providers in identifying TBI and associated co-occurring problems and determining potential need for further evaluation and/or mental health treatment modification.
Traumatic Brain Injury (TBI) is a significant public health concern. This toolkit provides mental health clinicians necessary information to address the needs of Veterans/Military Personnel with a history of TBI and co-occurring mental health conditions. Community mental health clinicians’ input was integral in identifying areas of focus. This toolkit is designed to assist providers in identifying TBI and associated co-occurring problems and determining potential need for further evaluation and/or mental health treatment modification.
The Purpose
 Between 2002 and 2012, approximately 1.8 million Veterans of the current conflicts in Afghanistan and Iraq left active duty and became eligible for health care through the Veterans Health Administration (VHA; Office of Public Health, 2014). Many of these Veterans are seeking medical and/or mental health care both within and outside of VHA. Approximately 59% of Operation Enduring Freedom/Operation Iraqi Freedom (OEF/OIF) Veterans have enrolled in VHA care (VHA; Office of Public Health, 2014), with the remainder either not seeking care or receiving it in the community.
Between 2002 and 2012, approximately 1.8 million Veterans of the current conflicts in Afghanistan and Iraq left active duty and became eligible for health care through the Veterans Health Administration (VHA; Office of Public Health, 2014). Many of these Veterans are seeking medical and/or mental health care both within and outside of VHA. Approximately 59% of Operation Enduring Freedom/Operation Iraqi Freedom (OEF/OIF) Veterans have enrolled in VHA care (VHA; Office of Public Health, 2014), with the remainder either not seeking care or receiving it in the community.
As such, community-based, non-VHA providers require the knowledge and skills to meet the specialized needs of this population.
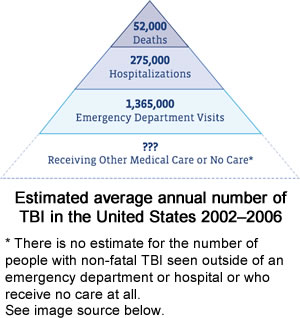
One area of need among OEF/OIF Veterans is related to TBI and co-occurring mental health concerns. Military personnel serving in Iraq and Afghanistan are sustaining injuries while deployed (Terrio et al. 2009). In fact, TBI has been identified as a "signature injury" of the recent conflicts (Tanielian and Jaycox, 2008). Additionally, this cohort is reporting a variety of psychiatric symptoms as well, including those associated with posttraumatic stress disorder (PTSD), depression (Tanielian and Jaycox, 2008), and substance use disorder (Seal et al., 2011).
The purpose of this toolkit is to offer providers working with Veterans who have a history TBI and mental health symptoms the following:
- Background information/Education
- Screening and Assessment Tools
- Interventions and Treatment Modification Suggestions
- Additional resources
This toolkit offers a useful starting point to increase the provision of TBI-related mental health services by community providers.
References
Bagalman, E. (2013). Mental disorders among OEF/OIF Veterans using VA health care: Facts and figures. Congressional Research Service.
Terrio, H., Brenner., L.A., Iwins, B.J., Cho, J.M., Helmick, K., Schwab, K., et al. (2009). Traumatic brain injury screening: Preliminary findings in a US Army brigade combat team. Journal of Head Trauma Rehabilitation, 24(1), 14-23.
Tanelian, T., & Jaycox, L.H. (Eds). (2008). Invisible wounds of war: Psychological and cognitive injuries, their consequences, and services to assist recovery. Santa Monica, CA: RAND Corporation.
Seal, K., Cohen, G., Waldrop, A., Cohen, B., Maquen, S., Ren, L. (2013). Substance use disorders in Iraq and Afghanistan veterans in VA healthcare, 2001-2010: Implications for screening, diagnosis and treatment. Drug Alcohol Dependency, 116(1-3), 93-101.
Image source: Faul M, Xu L, Wald MM, Coronado VG. Traumatic Brain Injury in the United States: Emergency Department Visits, Hospitalizations and Deaths 2002–2006. Atlanta (GA): Centers for Disease Control and Prevention, National Center for Injury Prevention and Control; 2010.
Structure of the Toolkit
This toolkit is divided into 4 sections, each containing background, screening, assessment and intervention information. For the purposes of this toolkit, screening, assessment and intervention are defined at right.
- Military/Veteran Culture- Provides the user with an orientation to Military/Veteran culture with information about topics such as the branches of the Armed Forces, the structure of the Department of Veterans Affairs, and resources regarding military culture.
- Behavioral Health/Co-occurring Psychiatric Conditions- Users will find information about symptoms and conditions that sometimes co-occur with TBI, such as substance use, depression, PTSD, and suicide risk.
- Traumatic Brain Injury- Contains information such as TBI severity classification, common sequelae, how to assess for TBI, and treatment modification recommendations.
- Resources- This section contains useful links to additional resources for Veterans, their support system and providers.
Reference
Myers, T. (2009). Mosby's Dictionary of Medicine, Nursing and Health Professions. St. Louis, MO: Mosby Elsevier.
Funding
This toolkit was developed as part of a collaborative project between the Veterans Integrated Service Network 19 Mental Illness Research, Education and Clinical Center (Rocky Mountain MIRECC) and the Colorado TBI Program at the Colorado Department of Human Services Division of Vocational Rehabilitation. The project is funded by the Health Resources and Services Administration (HRSA), the awarded grant number is H21MC21592, and with one aim being to increase the provision of mental health services to Veterans with TBI and co-occurring mental health concerns. The toolkit contains best practices identified at an expert consensus meeting, which were published in the Community Mental Health Journal (Olson-Madden, Brenner, Matarazzo, and Signoracci, 2013). The content is also based on input obtained from Colorado mental health providers who participated in focus groups aimed at identifying their learning needs regarding working with Veterans who have a history of TBI and co-occurring disorders (Matarazzo et al., under review).
References
Olson-Madden, J., Brenner, L., Matarazzo, B., & Signoracci, G. (2013). Identification and treatment of TBI and co-occurring psychiatric symptoms among OEF/OIF/OND veterans seeking mental health services within the state of Colorado: Establishing consensus for best practices. Community Mental Health Journal, 49(2), 220-229.
Matarazzo et al (under review). Community-based assessment and treatment of OEF/OIF/OND Veterans with a history of TBI and co-occurring mental health concerns: Using mixed methods to inform current practices, barriers and needs.
Sponsors:
Your Feedback
Your feedback is tremendously important to keeping this toolkit up to date and relevant. If you find broken links, out of date information, or you have questions, suggestions or quibbles please contact Joe Huggins at joe.huggins@va.gov.
Thanks!