CoE News - The Sleep Issue
Sleep, Suicide and Research for Veterans
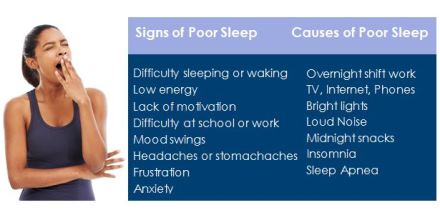
After a good night’s sleep, we feel rested, refreshed, and ready to take on the day. But after a poor night’s sleep, we may face the day tired, fatigued, irritable, and with less ability to focus. An estimated 70 million Americans are affected by lack of sleep and other sleeping disorders, making insufficient sleep a public health epidemic. Chronic lack of sleep has also been associated with certain physical and mental health disorders, such as diabetes, obesity, depression, anxiety, and as a growing body of evidence suggests, suicidal behavior. Sleep comes naturally for some but for others poor sleep can be caused by such sleep disorders as insomnia or sleep apnea. The Center of Excellence for Suicide Prevention (CoE), a Veterans Affairs (VA) research and education center, recognizes the need to address sleep disorders in the Veteran population. “We believe that poor sleep is an especially important risk factor for suicidal behavior because it affects so many Veterans.” says CoE Director, Dr. Ken Conner, “The good news is that there are effective treatments for sleep including behavioral treatments which have the advantage of teaching Veterans skills and strategies that they can use in their daily life. As a result, we are actively researching behavioral therapy treatments for Veterans with sleep problems who struggle with suicidal ideation or have a history of past suicide attempts in an effort to both improve sleep and reduce risk for these outcomes.”
The Big Picture from a Sleep Expert
Sleep expert Wilfred Pigeon, PhD, Chief of Clinical Research at the Veterans Affairs (VA) Center of Excellence for Suicide Prevention (CoE) and Associate Professor at the University of Rochester Medical Center leads the sleep and suicide studies for the CoE. We sat down with Dr. Pigeon to discuss sleep, suicide and his work.
Why is sleep an area of concern for the Department of Veterans Affairs?
Rates of sleep problems increase with age in everybody, and in the VA we have a lot of older veterans, so we tend to see a lot of sleep problems. We also have large numbers of Veterans returning from deployment. Many of these Veterans may have developed other mental health conditions. Insomnia in particular often co-occurs with PTSD and with depression and is quite common in people who have been exposed to traumatic events, regardless of whether they have developed PTSD. Because of these several contributing factors, there are a lot of sleep problems among Veterans. On the basis of a high prevalence of sleep problems alone, the VA is interested in addressing these problems to improve the health of Veterans. Beyond that, we’re beginning to show that when we treat a sleep problem, it can make other things better as well. If we treat insomnia, for instance, not only does insomnia get better, but the severity of depression can improve. Notably, the severity of depression decreases, even if we’re not directly treating the depression. Sleep apnea is another sleep disorder of interest to us. Again, because it is not uncommon and because the risk increases with age. In addition, when left untreated, sleep apnea can lead to all sorts of cardiovascular problems such as high blood pressure. In fact, treating sleep apnea can decrease the risk for heart attack and stroke. Finally, the VA is interested in sleep because it’s now identified as a risk factor for suicide. As I have noted, we know that we can improve sleep in persons with sleep disorders, so theoretically, if we can treat one of the risk factors for suicide, we can reduce the overall risk of suicide. So for all of those reasons the VA is very interested in addressing sleep problems.
What is the connection between suicide and sleep problems?
It may not seem like there would be a connection but if you think about how important sleep is to humans, it begins to make a lot of sense. Sleep is very important because it is rejuvenating, it’s refreshing, and it helps us function optimally during the day. Conversely if we’re not sleeping well, we’re not performing optimally; we’re a little tired, we’re a little irritable, we’re a little frustrated, and if that continues over time it becomes an additional stressor on our system. We don’t know precisely why there is a connection between sleep and suicidal thoughts and attempts and even death, but there is a connection. One thought is simply that poor sleep is an additional stressor, on top of many other stressors, that a person may have to deal with in their life. It might be the difference between having a very fleeting suicidal thought every once in a while, and having more chronic, persistent suicidal thoughts. It might be the difference between having suicidal thoughts and acting on those thoughts.
What questions are you looking to answer right now?
Is there something we can do to decrease suicidal thoughts? Can we improve sleep and thereby alleviate suicidal thoughts? So one of the ways that we’re trying to address this is to do studies on people who have suicidal thoughts and sleep problems. We try to treat their sleep problems then observe whether the severity of their suicidal thoughts decrease over time. If we can alleviate their suicide thoughts, then there’s a chance that their risk of suicide may be lessened.
Do you have any advice for providers and VA suicide prevention coordinators (SPCs)?
First ask Veterans about their sleep. You could ask if they are having trouble falling asleep or staying asleep. If so, that is probably insomnia and you might want to put that on their problem list, or directly refer them to someone in your facility that does Cognitive Behavioral Therapy for insomnia (CBT-I). You could ask them if they are having trouble sleeping, and if they say yes, you could ask them if they are snoring loudly and if anyone has ever said that they have paused during their breathing. In that case you should ask their primary care provider to “Please consider evaluation for sleep apnea”. So the role of the SPC with respect to sleep and their suicide prevention capacity would be to first assess whether there is a sleep problem, and begin to discern what kind of sleep problem may be present, particularly if it’s insomnia or nightmares or sleep apnea - kind of the big three at the VA. Depending on what they suspect, the SPC can make sure there is a referral in place for further evaluation.
A Good Night’s Sleep / Cognitive Behavioral Therapy for insomnia (CBT-I)
The best plan for Veterans experiencing trouble sleeping is to consult with a clinical provider who can determine if a sleep study is needed and whether Sleep Apnea, Insomnia or another underlying factor is responsible for the interrupted sleep. Different treatments will be used depending on the individual and the cause. Working with a provider gives one access to a number of treatments and interventions that can create optimal sleeping conditions.
Veterans Affairs (VA) has produced trainings for these sleep interventions. The Cognitive Behavioral Therapy for Insomnia (CBT-I) training is one of the national rollouts that the VA has recently done and is available to VA providers who see insomnia patients. There is also a VA App available, CBT-i Coach, which is meant to be used by patients in collaboration with their providers.
Cognitive Behavioral Therapy for Insomnia (CBT-I) involves working with patients to identify and then restructure negative beliefs and habits that may be prohibiting them from getting good quality sleep. Patients keep a sleep diary so that problems can be identified and progress can be measured. One of the main components of the process involves reversing negative associations between the bed or sleep environment and wakefulness by having the bed be associated only with sleep. CBT-I interventions can also involve improvements to the sleep environment, the creation of a set prebedtime routine, and various other forms of sleep hygiene.
CoE People - Dr. Todd Bishop by Emily Smith

Todd Bishop, PhD, knew early in his undergraduate training that he wanted to become a clinical psychologist. Upon completion of his PhD at the University of Syracuse in 2014, Todd joined the VA VISN 2 Center of Excellence for Suicide Prevention (CoE) as a Postdoctoral Fellow where his time is split between clinical work and research.
Dr. Bishop’s background serving in the Army National Guard and working in a New York City sleep lab as a polysomnographic technician has made for an ideal segue into his current work examining the relationship between disrupted sleep patterns and suicidal behavior in Veterans. Dr. Bishop, in ongoing research with his mentor and CoE Director of Clinical Research, Dr. Wilfred Pigeon, evaluates Cognitive Behavioral Therapy for Insomnia (CBT-I) interventions in a population of Veterans suffering from insomnia, depression or PTSD, and suicide ideation or behaviors. “This work is an opportunity to give back to the Veteran community.” says Dr. Bishop. And although each Veteran brings an individual story of service, Dr. Bishop has found that his background guides him in conducting therapy sessions and designing research questions for this unique population.
The Veteran population is often affected by significant risk factors for suicide, some of which include: chronic illness and pain, depression, and substance use. However, beyond the most commonly recognized, Dr. Bishop emphasizes that sleep problems are a factor on their own, “even after accounting for other factors, insomnia still independently indicates a higher risk of suicidal actions.” he says. The idea that insomnia and other forms of disrupted sleep can indicate a higher risk for suicidal behavior could also apply to shift workers of all types. Bishop recalls from his own experiences “I never drank coffee before I joined the Army…and now I live on coffee.” He remembers how the wake/sleep cycle of a Servicemember can mirror that of other shift workers, such as chefs and firefighters, who work odd hours that can disrupt circadian rhythm and impede sleep.
Dr. Bishop has been pleasantly surprised by how quickly some Veterans report an improvement in their sleep patterns following CBT-I interventions. “It’s like hitting the reset button on your brain and body in terms of sleep,” he says, “the first couple of weeks are the most difficult…but gradually people notice the difference.” He also notes “when people get better, they tend to get better quickly.” Through this research, Dr. Bishop hopes to continue helping Veterans to improve their quality of sleep and, by extension, quality of life.
About CoE
CoE is dedicated to Research & Education on Suicide Prevention and identifying measures to save Veteran lives. Director: Dr. Ken Conner Associate Director & Director of Education: Dr. Jan Kemp. To learn more go to http://www.mirecc.va.gov/suicideprevention/index.asp
CoE News August 2015 Editor: Jan Kemp, RN, PhD
Writer: Rachel Warden unless otherwise noted.
Subscribe to CoE News


















