VA, VISN 20, and NW MIRECC History
VA, VISN 20, and NW MIRECC History
 Supporting, caring for, and honoring Veterans is woven into the fabric of the United States. From the earliest days of American history, soldiers and members of the militia were wounded in service or died, leaving widows and orphans with no financial support. Care for disabled service members and dependents fell to colonies, states, and eventually the federal government. The origins of the United States Department of Veterans Affairs (VA) date back to 1636 with the Pilgrims in Plymouth Colony. During their conflict with the Pequot Indians, the Pilgrims enacted a law ensuring that disabled soldiers would receive support from the colony. Responsibility for caring for disabled service members and their dependents initially lay with colonies and states before eventually becoming a federal government duty. From the early days of American history, soldiers and militiamen wounded in action or deceased often left behind widows and orphans without financial backing. The first shots of what would evolve into the American War of Independence were fired in April 1775. Although the American colonies had depended on the militia system for 150 years, in June 1775, the Second Continental Congress sanctioned the formation of a Continental Army, appointing George Washington as commander in chief.
Supporting, caring for, and honoring Veterans is woven into the fabric of the United States. From the earliest days of American history, soldiers and members of the militia were wounded in service or died, leaving widows and orphans with no financial support. Care for disabled service members and dependents fell to colonies, states, and eventually the federal government. The origins of the United States Department of Veterans Affairs (VA) date back to 1636 with the Pilgrims in Plymouth Colony. During their conflict with the Pequot Indians, the Pilgrims enacted a law ensuring that disabled soldiers would receive support from the colony. Responsibility for caring for disabled service members and their dependents initially lay with colonies and states before eventually becoming a federal government duty. From the early days of American history, soldiers and militiamen wounded in action or deceased often left behind widows and orphans without financial backing. The first shots of what would evolve into the American War of Independence were fired in April 1775. Although the American colonies had depended on the militia system for 150 years, in June 1775, the Second Continental Congress sanctioned the formation of a Continental Army, appointing George Washington as commander in chief.
On 14 June 1775, Congress "Resolved, That six companies of expert riflemen, be immediately raised in Pennsylvania, two in Maryland, and two in Virginia [and] as soon as completed, shall march and join the army near Boston, to be there employed as light infantry, under the command of the chief Officer in that army." On 13 October 1775, the Continental Congress marked the establishment of what is now the United States Navy, "Resolved, That a swift sailing vessel, to carry ten carriage guns, and a proportionable number of swivels, with eighty men, be fitted, with all possible despatch, for a cruise of three months, and that the commander be instructed to cruize eastward, for intercepting such transports as may be laden with warlike stores and other supplies for our enemies, and for such other purposes as the Congress shall direct." The Continental Navy, created during the War of Independence called for "a swift sailing vessel, to carry ten carriage guns, and a proportionable number of swivels, with eighty men, be fitted, with all possible despatch, for a cruise of three months...". The Constitution of the United States, ratified in 1789, empowered Congress "to provide and maintain a Navy." On November 10, 1775, the Second Continental Congress formed two battalions of Continental Marines.
In 1776, the Continental Congress encouraged enlistments during the Revolutionary War by offering pensions to disabled soldiers. General George Washington introduced the "Badge of Merit" on August 7, 1782, which greatly influenced the design and significance of today's Purple Heart. Although Native Americans were not extended citizenship rights until 1924, Native Americans have served the United States with honor, loyalty, and bravery since the Revolutionary War. Following the War of Independence, the Continental Navy's ships were sold, and both sailors and officers were dismissed. Similarly, after their contributions to the American Revolution, the Marines were disbanded after the Treaty of Paris in April 1783. During the American Revolution, the Continental Congress passed the first national pension laws for wounded or injured soldiers but left it to the states to distribute relief. After 1789, the federal government assumed responsibility for pensions.
 In Septemeber of 1789, Congress passed a resolution asking that the President of the United States recommend to the nation a day of thanksgiving for "sincere and humble thanks". A few days later, President George Washington issued a proclamation naming Thursday, November 26, 1789 as a "Day of Publick Thanksgivin". On October 3, 1863, President Lincoln declared the traditional Thanksgiving celebration a nationwide holiday to be observed each year on the fourth Thursday of November. The origin of the American Thanksgiving tradition of feasting, though, is generally credited to the Pilgrims. As early as 1621, the Puritan colonists of Plymouth, Massachusetts set aside a day of thanks for a bountiful harvest. Throughout the colonial period and into the nineteenth century, official days of feasting and fasting commemorated periods of good and poor fortune. While most proclaimed Thanksgiving for the fourth or last Thursday of November, Franklin D. Roosevelt chose the third Thursdays of November 1939 through 1941, for economic reasons. Late in 1941, Congress passed Thanksgiving legislation that Roosevelt signed into law on December 26, 1941. Public Law 77-379 set Thanksgiving Days from 1942 onward to the fourth Thursday in November. The law also made Thanksgiving Day an annual Federal Holiday.
In Septemeber of 1789, Congress passed a resolution asking that the President of the United States recommend to the nation a day of thanksgiving for "sincere and humble thanks". A few days later, President George Washington issued a proclamation naming Thursday, November 26, 1789 as a "Day of Publick Thanksgivin". On October 3, 1863, President Lincoln declared the traditional Thanksgiving celebration a nationwide holiday to be observed each year on the fourth Thursday of November. The origin of the American Thanksgiving tradition of feasting, though, is generally credited to the Pilgrims. As early as 1621, the Puritan colonists of Plymouth, Massachusetts set aside a day of thanks for a bountiful harvest. Throughout the colonial period and into the nineteenth century, official days of feasting and fasting commemorated periods of good and poor fortune. While most proclaimed Thanksgiving for the fourth or last Thursday of November, Franklin D. Roosevelt chose the third Thursdays of November 1939 through 1941, for economic reasons. Late in 1941, Congress passed Thanksgiving legislation that Roosevelt signed into law on December 26, 1941. Public Law 77-379 set Thanksgiving Days from 1942 onward to the fourth Thursday in November. The law also made Thanksgiving Day an annual Federal Holiday.
In the final decade of the 20th century, VA Medical Centers were reorganized into 22 Veterans Integrated Service Networks (VISNs). Currently, 18 VISNs function as regional care systems to better address local health care needs and enhance access to treatment. In the Pacific Northwest, VISN 20 serves Veterans in Alaska, Oregon, Washington, most of Idaho, and one county each in Montana and California. Operating across three time zones over 817,417 square miles, VISN 20 is home to 273 federally recognized American Indian and Alaskan Native tribes. Spanning 23% of US land mass, VISN 20 is the largest geographic region of VA. According to the United States Department of Defense (DoD), American Indians and Alaska Natives have one of the highest representations in the U.S. Armed Forces. VA consults with American Indian and Alaska Native tribal governments to develop partnerships that enhance access to services and benefits by Veterans and their families. VA is committed to ensuring that Native American Veterans and their families are able to utilize all benefits and services they are entitled to receive. As of the end of FY2024, 39% of VISN 20 enrollees resided in rural or highly rural areas.
In the year 1794 Congress first acted on that power, in response to international crises, by authorizing the procuring and manning of six frigates. President Washington signed the "Act to provide a Naval Armament" on March 27, 1794 authorizing authorizing construction of the Navy’s first six frigates; USS United States (launched 1797), USS Constellation (1797), USS Constitution (1797), USS Congress (1799), USS Chesapeake (1799), and USS President (1800). Congress established the Department of the Navy in April 1798. After the American War of Independence, the newly established U.S. Constitution granted Congress the authority “to provide and maintain a navy.” Originating during the American Revolution, the U.S. Navy has transformed from a fleet of sail and steam-powered ships into a high-tech fleet with nuclear-powered vessels and supersonic aircraft.
In July 1798, Congress reestablished the United States Marine Corps for service under the Secretary of the Navy. This corps included "one major, four captains, sixteen first lieutenants, twelve second lieutenants, forty-eight sergeants, forty-eight corporals, thirty-two drums and fifes, and seven hundred and twenty privates, including the marines who have been enlisted, or are authorized to be raised for the naval armament," and was organized into as many companies or detachments as directed by the President. While Marines initially served as landing forces for the naval fleet, their role has significantly expanded over more than two centuries. Today, they also guard U.S. embassies worldwide and act as rapid deployment forces to stabilize conflict areas until reinforcements arrive.
 In the Republic's formative years, direct medical and hospital care for Veterans was provided by individual states and communities. President John Adams established U.S. Marine Hospitals through the 1798 "Act for the Relief of Sick and Disabled Seamen". Seamen began paying for the U.S. Marine Hospitals through a deduction of monthly wages providing the Federal Government with a fund for medical services at U.S. Marine Hospitals and construction of new hospitals. The first U.S. Marine Hospital purchased and owned by the Federal Government was in the State of Virginia (Washington Point) in Norfolk County. In the Pacific Northwest, notable U.S. Marine Hospitals were located in Seattle, Port Townsend/Port Angeles, Knappton Cove, and Portland. Boston Harbor was the location of the first Marine Hospital on the peninsula of Castle Island. In 1804, the Castle Island Marine Hospital was relocated northeast to the Charlestown section of Boston.In the early 1800's, President Thomas Jefferson purchased the Louisiana territory from France. President Jefferson ordered exploration beyond "great rock mountains" and formed the Corps of Discovery led by Meriwether Lewis and William Clark. The two-year journey was a successful search of a water link between the Columbia and Missouri rivers when in 1805, Lewis and Clark reached the Pacific Ocean. The Corps of Discovery would lead diplomatic relations with Chinook Indians and set winter from 1805-1806 at Fort Clatsop. The diplomacy with Native American tribes forged a pathway in what would eventually become the contiguous 48 United States.
In the Republic's formative years, direct medical and hospital care for Veterans was provided by individual states and communities. President John Adams established U.S. Marine Hospitals through the 1798 "Act for the Relief of Sick and Disabled Seamen". Seamen began paying for the U.S. Marine Hospitals through a deduction of monthly wages providing the Federal Government with a fund for medical services at U.S. Marine Hospitals and construction of new hospitals. The first U.S. Marine Hospital purchased and owned by the Federal Government was in the State of Virginia (Washington Point) in Norfolk County. In the Pacific Northwest, notable U.S. Marine Hospitals were located in Seattle, Port Townsend/Port Angeles, Knappton Cove, and Portland. Boston Harbor was the location of the first Marine Hospital on the peninsula of Castle Island. In 1804, the Castle Island Marine Hospital was relocated northeast to the Charlestown section of Boston.In the early 1800's, President Thomas Jefferson purchased the Louisiana territory from France. President Jefferson ordered exploration beyond "great rock mountains" and formed the Corps of Discovery led by Meriwether Lewis and William Clark. The two-year journey was a successful search of a water link between the Columbia and Missouri rivers when in 1805, Lewis and Clark reached the Pacific Ocean. The Corps of Discovery would lead diplomatic relations with Chinook Indians and set winter from 1805-1806 at Fort Clatsop. The diplomacy with Native American tribes forged a pathway in what would eventually become the contiguous 48 United States.
Also in the early 1800s, a small office of three in the War Department handled the clerical work relating to claims and the few thousand Veterans on the pension rolls. In 1811, the U.S. Navy petitioned Congress to enact legislation for establishing a Home in Philadelphia to support "destitute Navy sailors and Marines." An interim Naval Hospital was set up in the erstwhile country mansion of the esteemed Pemberton family in Philadelphia. On April 3, 1827, Commodore William Bainbridge oversaw the cornerstone laying of the U.S. Naval Asylum. In his dedication speech, Bainbridge declared, "A home will be established for the faithful (seaman) who has been worn out or maimed in fighting the battles of his country. A comfortable harbor will be secured where he may safely moor and ride out the ebb of life free from cares and storms, by which he has been previously surrounded." It would take until 1831 for the Naval Asylum to become operational with four regular inmates. Founded in 1834, the U.S. Naval Asylum was America’s first federal retirement facility for veterans. Fully funded by Navy appropriations, the institution's name was changed to the United States Naval Home in 1889 and was home to U.S. Navy pensioners and retirees. The U.S. Naval Home continued operation in Philadelphia until 1976 when the home was relocated to Mississippi.
 Congress authorized the United States Soldiers' Home in 1851. Historically, the Soldiers Home was funded by monthly contributions from enlisted personnel and warrant officers of the active-duty U.S. Army, and later the U.S. Air Force, as well as fines and forfeitures resulting from disciplinary actions. President Abraham Lincoln enjoyed visiting the United States Soldiers Home, along with his predecessors. As it expanded, he requested to use the cottage as a summer retreat to escape Washington D.C.'s humidity and political pressures. Lincoln spent approximately one-quarter of his presidency at the cottage, including while drafting the Emancipation Proclamation. President Lincoln's Cottage, part of the U.S. Military Asylum—The Old Soldiers’ Home (now known as the Armed Forces Retirement Home)—located at the corner of Upshur Street and Rock Creek Church Road NW in Washington, DC, has been recognized as a National Historic Landmark. The U.S. Naval Home with the U.S. Soldiers’ and Airmen’s Home were merged by the U.S. Congress in 1991 and named Armed Forces Retirement Home (AFRH). AFHR continues operation in both Gulfport, Mississippi and Washington, DC. Restoration of President Lincoln's Cottage at the Old Soldiers Home (AFHR) began in 2001, and it was opened to the public for the first time in history on President's Day in 2008.
Congress authorized the United States Soldiers' Home in 1851. Historically, the Soldiers Home was funded by monthly contributions from enlisted personnel and warrant officers of the active-duty U.S. Army, and later the U.S. Air Force, as well as fines and forfeitures resulting from disciplinary actions. President Abraham Lincoln enjoyed visiting the United States Soldiers Home, along with his predecessors. As it expanded, he requested to use the cottage as a summer retreat to escape Washington D.C.'s humidity and political pressures. Lincoln spent approximately one-quarter of his presidency at the cottage, including while drafting the Emancipation Proclamation. President Lincoln's Cottage, part of the U.S. Military Asylum—The Old Soldiers’ Home (now known as the Armed Forces Retirement Home)—located at the corner of Upshur Street and Rock Creek Church Road NW in Washington, DC, has been recognized as a National Historic Landmark. The U.S. Naval Home with the U.S. Soldiers’ and Airmen’s Home were merged by the U.S. Congress in 1991 and named Armed Forces Retirement Home (AFRH). AFHR continues operation in both Gulfport, Mississippi and Washington, DC. Restoration of President Lincoln's Cottage at the Old Soldiers Home (AFHR) began in 2001, and it was opened to the public for the first time in history on President's Day in 2008.
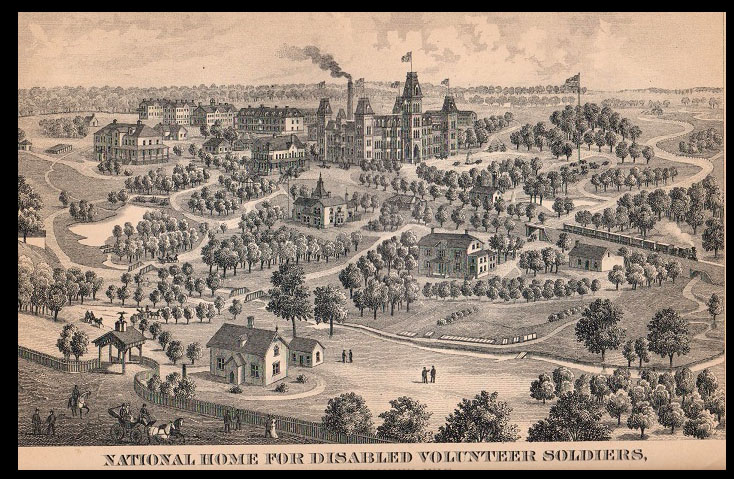
In 1865, Senator Henry Wilson, chairman of the Senate Committee on Military Affairs and the Militia, introduced a bill to "incorporate a National Military and Naval Asylum for the relief of the totally disabled officers and men of the volunteer forces of the United States". On March 3, 1865, one month before the Civil War concluded, President Lincoln approved the establishment of the National Asylum for Disabled Volunteer Soldiers through "An Act to Incorporate a National Military and Naval Asylum for the Relief of the Totally Disabled Officers and Men of the Volunteer Forces of the United States". This asylum was pioneering in providing civilian medical care to Veterans of temporary volunteer forces globally. While the U.S. Naval and Soldiers Homes catered to retired members of the Regular Navy and Army, volunteer soldiers' homes run by the federal government were not established until after the Civil War. Previously, two smaller soldiers' homes operated by the U.S. Army and Navy for Veterans of the Regular military forces each accommodated up to 300 men. The National Homes, however, housed tens of thousands of Veterans and were commonly referred to as “soldiers’ homes” or “military homes.”

In 1866, Congress passed new legislation lowering the number of board managers of the asylum. From 1866 to 1930, NHDVS opened branches nationwide, establishing eleven regional campuses with cemeteries that provided comprehensive domiciliary and medical care, forming the foundation of the VA's Veterans Health Administration (VHA). Originally conceived as the first government institution dedicated solely to honorably discharged volunteer soldiers, in 1873 Congress changed the name from National Asylum for Disabled Volunteer Soldiers to the National Home for Disabled Volunteer Soldiers (NHDVS). NHDVS provided relief of the totally disabled officers and men of the volunteer forces of the United States. Numerous current VA hospitals and medical centers originated as National Homes, Public Health Service, U.S. Marine Hospitals, or Veterans Bureau Hospitals. Through 1874, NHDVS was funded by fines and forfeitures imposed by court-martial and forfeitures on account of desertions. Congress funded NHDVS from 1875 to 1931. The NHDVS network of residential facilities were located in Togus, Maine (Togus VA Medical Center); Dayton, Ohio (Dayton VA Medical Center); Wood, Wisconsin (Clement J. Zablocki VA Medical Center); Hampton, Virginia (Hampton VA Medical Center); Leavenworth, Kansas (Dwight D. Eisenhower Department of Veterans Affairs Medical Center); Sawtelle, California (West Los Angeles VA Medical Center); Marion, Indiana (Marion VA Medical Center); Roseburg, Oregon (Roseburg VA Medical Center); Danville, Illinois (Danville VA Medical Center); Johnson City, Tennessee (James H. Quillen Department of Veterans Affairs Medical Center); Hot Springs, South Dakota (Hot Springs VA Medical Center); Bath, New York (Bath VA Medical Center), and St. Petersburg, Florida (C.W. Bill Young Department of Veterans Affairs Medical Center).
Opened in 1855, Government Hospital for the Insane, was the first federally funded mental institution. The Government Hospital for the Insane was founded “to provide the most humane care and enlightened curative treatment of the insane of the Army, Navy and the District of Columbia.” In 1882, Congress authorized transfer of military personnel from NHDVS mental wards to the Government Hospital for the Insane. During the Civil War, buildings of the Government Hospital for the Insane were used by the Union army and navy wounded. The hospital was renamed in 1916, St. Elizabeth's Hospital. In 2003, the west campus ceased operation and become the headquarters of the United States Department of Homeland Security. The District of Columbia, Department of Behavioral Health took over the East campus in 2010.
 Idaho would become part of the Washington territory after Oregon was granted statehood in 1859. The Idaho territory was born 1863 and would include land that would then become Montana and Wyoming. Established in June 1863, Fort Boise was renamed Boise Barracks in 1879. Idaho would become the 43rd state in July of 1890. On February 7, 1938, an Executive Order facilitated the transfer of 110 acres of Boise Barracks Military Reservation from the War Department to the control and jurisdiction of the Veteran's Administration. A. Since 1950, the Boise VA Medical Center has occupied the primary area of the former Fort Boise grounds. Besides early settlers' 1863 log cabins preserved as historical artifacts, the oldest buildings in Boise were constructed for the Fort. Military units continued to safeguard the citizens of Boise and southwestern Idaho until the Fort's formal abandonment in 1912. Soldiers briefly returned in 1916 for the Mexican border campaign preparation. The Idaho State Veterans Home in Boise operates on land transferred from the VA. The Idaho State Soldiers' Home opened in 1895. Additional Idaho State Veterans Homes are located in Lewiston, Pocatello, and Post Falls. The sandstone buildings erected in 1864 are still utilized by the Boise VA Medical Center today. The VA's Boise Healthcare System delivers health care services to Veterans at six locations in Idaho and eastern Oregon. These VHA Boise facilities include the Boise VA Medical Center and five VHA Community Based Outpatient Clinics (CBOCs) in Caldwell, Mountain Home, Salmon, and Twin Falls, Idaho, and Hines, Oregon. The 40-acre Idaho State Veterans Cemetery – Blackfoot serves more than 20,000 eastern Idaho veterans and their families. In 2000, Idaho's Division of Veterans Services was stood up and four years later, the Idaho State Veterans Cemetery opened in Boise, Idaho.
Idaho would become part of the Washington territory after Oregon was granted statehood in 1859. The Idaho territory was born 1863 and would include land that would then become Montana and Wyoming. Established in June 1863, Fort Boise was renamed Boise Barracks in 1879. Idaho would become the 43rd state in July of 1890. On February 7, 1938, an Executive Order facilitated the transfer of 110 acres of Boise Barracks Military Reservation from the War Department to the control and jurisdiction of the Veteran's Administration. A. Since 1950, the Boise VA Medical Center has occupied the primary area of the former Fort Boise grounds. Besides early settlers' 1863 log cabins preserved as historical artifacts, the oldest buildings in Boise were constructed for the Fort. Military units continued to safeguard the citizens of Boise and southwestern Idaho until the Fort's formal abandonment in 1912. Soldiers briefly returned in 1916 for the Mexican border campaign preparation. The Idaho State Veterans Home in Boise operates on land transferred from the VA. The Idaho State Soldiers' Home opened in 1895. Additional Idaho State Veterans Homes are located in Lewiston, Pocatello, and Post Falls. The sandstone buildings erected in 1864 are still utilized by the Boise VA Medical Center today. The VA's Boise Healthcare System delivers health care services to Veterans at six locations in Idaho and eastern Oregon. These VHA Boise facilities include the Boise VA Medical Center and five VHA Community Based Outpatient Clinics (CBOCs) in Caldwell, Mountain Home, Salmon, and Twin Falls, Idaho, and Hines, Oregon. The 40-acre Idaho State Veterans Cemetery – Blackfoot serves more than 20,000 eastern Idaho veterans and their families. In 2000, Idaho's Division of Veterans Services was stood up and four years later, the Idaho State Veterans Cemetery opened in Boise, Idaho.
In 1861, the Congressional legislation introduced the creation of the medal of honor to "promote efficiency of the Navy" for enlisted seamen and marines who "distinguish themselves by gallantry in action and other seamenlike qualities" during the Civil War. President Lincoln signed the legislation on December 21, 1861. Lincoln signed legislation the following year for the Army Medal of Honor for non-commisioned officers and privates. Army officers became eligible in 1863 and Navy officers later in 1915. The Congressional Medal of Honor Society was chartered in 1958 through the signature of President Dwight Eisenhower. New guidelines for awarding the Medal of honor were released in 1963, "while engaged in an action against an enemy of the United States,...while engaged in military operations involving a conflict with an opposing foreign force,...or while serving with friendly forces in an armed conflict against an opposing armed force in which the United States in not a belligerent party".
 Throughout the years, the Medal of Honor has gone through legislative, design and presentation changes while remaining the highest award for military valor in action serving the U.S. Armed Forces. President Theodore Roosevelt is the only president to be awarded the Medal of Honor. On July 1, 1898, in San Juan Hill, Cuba, Lieutenant Colonel Roosevelt was serving with the 1st U.S. Volunteer Cavalry Regiment (Rough Riders); "For conspicuous gallantry and intrepidity at the risk of his life above and beyond the call of duty, Lieutenant Colonel Theodore Roosevelt distinguished himself by acts of bravery on 1 July 1898, near Santiago de Cuba, Republic of Cuba, while leading a daring charge up San Juan Hill. Lieutenant Colonel Roosevelt, in total disregard for his personal safety, and accompanied by only four or five men, led a desperate and gallant charge up San Juan Hill, encouraging his troops to continue the assault through withering enemy fire over open countryside. Facing the enemy's heavy fire, he displayed extraordinary bravery throughout the charge, and was the first to reach the enemy trenches, where he quickly killed one of the enemy with his pistol, allowing his men to continue the assault. His leadership and valor turned the tide in the battle for San Juan Hill. Lieutenant Colonel Roosevelt's extraordinary heroism and devotion to duty are in keeping with the highest traditions of military service and reflect great credit upon himself, his unit, and the United States Army". In 2013, the United States Congress set new time limits for the Medal of Honor: "recommendations must be made within three years of the valorous action and the medal must be presented within five years".
Throughout the years, the Medal of Honor has gone through legislative, design and presentation changes while remaining the highest award for military valor in action serving the U.S. Armed Forces. President Theodore Roosevelt is the only president to be awarded the Medal of Honor. On July 1, 1898, in San Juan Hill, Cuba, Lieutenant Colonel Roosevelt was serving with the 1st U.S. Volunteer Cavalry Regiment (Rough Riders); "For conspicuous gallantry and intrepidity at the risk of his life above and beyond the call of duty, Lieutenant Colonel Theodore Roosevelt distinguished himself by acts of bravery on 1 July 1898, near Santiago de Cuba, Republic of Cuba, while leading a daring charge up San Juan Hill. Lieutenant Colonel Roosevelt, in total disregard for his personal safety, and accompanied by only four or five men, led a desperate and gallant charge up San Juan Hill, encouraging his troops to continue the assault through withering enemy fire over open countryside. Facing the enemy's heavy fire, he displayed extraordinary bravery throughout the charge, and was the first to reach the enemy trenches, where he quickly killed one of the enemy with his pistol, allowing his men to continue the assault. His leadership and valor turned the tide in the battle for San Juan Hill. Lieutenant Colonel Roosevelt's extraordinary heroism and devotion to duty are in keeping with the highest traditions of military service and reflect great credit upon himself, his unit, and the United States Army". In 2013, the United States Congress set new time limits for the Medal of Honor: "recommendations must be made within three years of the valorous action and the medal must be presented within five years".
In the late 1800s, National and State Homes were established in Idaho, Oregon, and Washington. Washington was granted statehood in November 1889. Washington state Session Laws of 1907, HB #9, which included the Enabling Act to establish the Washington Veterans’ Home was passed by the State Legislature and signed by Governor Albert E. Mead. The first Soldiers' Home in the Pacific Northwest was located in Orting, Washington. Every National Home included a hospital, barracks, dining hall, recreational facilities, and a cemetery. In 1907, Washington passed legislation to establish the Washington Veterans' Home in Retsil. Overlooking Sinclair Inlet in Kitsap County, the Washington Veterans Home at Port Orchard (Retsil) was built on 31 acres in 1910.
The origin of the VA's National Cemetery Administration (NCA) begins with the Civil War and President Abraham Lincoln. In 1862, Congress authorized President Lincoln to enact legislation that authorized Lincoln “to purchase cemetery grounds…to be used as a national cemetery for the soldiers who shall die in the service of the country”. After the war, the National Cemetery Act of February 22, 1867, was the first law to finance and develop national cemeteries through the acquisition of land, buildings, walls, and permanent upright marble headstones. NCA is one of three federal agencies responsible for managing national cemeteries in the United States. Its mission includes the oversight of most national cemeteries and the provision of grave markers for qualified Veterans. In Oregon, Fort Stevens was authorized by Congress in 1862. The Quartermaster of Fort Stevens received authority to construct a cemetery four years later. The 273 headstones of Fort Stevens National Cemetery recalls patriotism, heroism, and service. Additionally, during the 19th century, the nation's Veterans assistance program was broadened to include benefits and pensions for not only Veterans but also their widows and dependents.
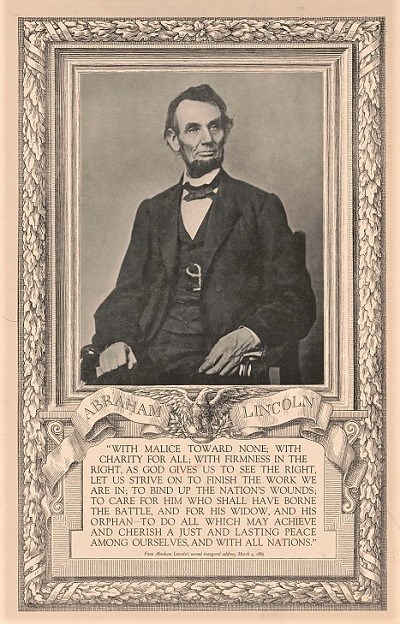 In the closing weeks of the Civil War, President Lincoln stood at the East Portico of the U.S. Capitol to deliver his second inaugural address. He concluded his speech with a poignant appeal for healing and reconciliation, accompanied by a solemn vow to those who had labored to reunite the nation: "With malice toward none; with charity for all; with firmness in the right, as God gives us to see the right, let us strive on to finish the work we are in; to bind up the nation’s wounds; to care for him who shall have borne the battle, and for his widow, and his orphan—to do all which may achieve and cherish a just and a lasting peace, among ourselves, and with all nations".
In the closing weeks of the Civil War, President Lincoln stood at the East Portico of the U.S. Capitol to deliver his second inaugural address. He concluded his speech with a poignant appeal for healing and reconciliation, accompanied by a solemn vow to those who had labored to reunite the nation: "With malice toward none; with charity for all; with firmness in the right, as God gives us to see the right, let us strive on to finish the work we are in; to bind up the nation’s wounds; to care for him who shall have borne the battle, and for his widow, and his orphan—to do all which may achieve and cherish a just and a lasting peace, among ourselves, and with all nations".
Memorial Day, originally known as Decoration Day, began to be observed by numerous communities post-Civil War, a conflict that resulted in over 620,000 military fatalities, representing about 2 percent of the population at the time. The tradition of Decoration Day emerged in the 1860s when both Northern and Southern groups started placing flowers on the graves of Civil War soldiers who had perished. The Grand Army of the Republic (GAR), an organization of Union veterans, officially instituted Decoration Day in 1868. On May 30, 1868, more than 5,000 people convened at Arlington National Cemetery for the inaugural Decoration Day (now known as Memorial Day) event. Before adorning the soldiers' graves with flowers, President James Abram Garfield, an Ohio congressman and former Union major general, addressed the crowd. In his maiden address at Arlington National Cemetery, and others nationwide, Garfield emphasized the essence and significance of commemorating Decoration Day. The GAR designated May 30 for the ceremony to ensure the availability of "the choicest flowers of springtime" across the country. "No specific form or ceremony is mandated, but posts and comrades will arrange appropriate services and respects as circumstances allow." Typical programs featured parading veterans, ceremonies involving flags, music, and prayers, with flower-adorned graves attended by families and the public.
Over the ensuing decades, the term Memorial Day began to replace or accompany Decoration Day, especially after World War I, broadening to honor Veterans from all wars, not just the Civil War. In 1967, the U.S. Congress confirmed "Memorial Day" as the official name of the holiday. Many people confuse Memorial Day and Veterans Day. Memorial Day is a day for remembering and honoring military personnel who died in the service of their country, particularly those who died in battle or as a result of wounds sustained in battle. While those who died are also remembered, Veterans Day is the day set aside to thank and honor all those who served honorably in the military – in wartime or peacetime. In fact, Veterans Day is largely intended to thank living Veterans for their service, to acknowledge that their contributions to our national security are appreciated, and to underscore the fact that all those who served – not only those who died – have sacrificed and done their duty. Today, Memorial Day is a designated annual day to honor all individuals who have died in service to the United States during times of war and peace. The "National Moment of Remembrance Act" encourages all Americans to pause at 3:00 p.m. local time for a moment of silence to reflect upon those who have sacrificed their lives in service to the country. In 1971, Congress declared Memorial Day a national holiday to be observed on the last Monday in May.
 In 1867, the Russians sold Alaska to the United States for $7.2 million and a transfer ceremony took place in Sitka on October 18. Although the U.S. flag first flew over Alaska in 1867, it was not until the 1884 passage of the first Organic Act establishing the region as "a civil and judicial district" that Congress provided any form of government. Though the U.S. Air Force became an independent entity of the DoD on September 18, 1947, its roots trace back to the early 1900s when the Army Signal Corps founded an Aeronautic Division in 1907. In 1915, the U.S. Lifesaving Service combined with the Revenue Cutter Service (Revenue Marine Service) to form the United States Coast Guard. The U.S. Coast Guard recognizes August 4, 1790, as the service birthday (Coast Guard Day) when Congress approved Secretary of the Treasury Alexander Hamilton's proposal to construct ten cutters establishing the Revenue Marine Service. In 1924, when Sitka National Cemetery was designated, most of the interments were soldiers and sailors from the Marine base and Naval hospital. Since then, there have been several acreage modifications: in 1925, a revision of the executive order reduced the acreage from 3.98 acres to 1.19 acres; in 1957, Sheldon Jackson Junior College donated approximately one acre; a donation of 0.20 acres was made in 1959 by the Board of National Missions of the Presbyterian Church of the United States; and the Department of Interior transferred approximately two acres in the mid-1980s. Sitka National Cemetery currently encompasses 4.3 acres. The remote Sitka National Cemetery is located half a mile east of the center of town and is dominated by the natural beauty of the mountains and waters of Sitka Bay. The only access to Sitka is by air, marine highway or weekly ferry from Seattle, WA. In Alaska, the Metlakatla Veterans Cemetery officially opened in July of 2022.
In 1867, the Russians sold Alaska to the United States for $7.2 million and a transfer ceremony took place in Sitka on October 18. Although the U.S. flag first flew over Alaska in 1867, it was not until the 1884 passage of the first Organic Act establishing the region as "a civil and judicial district" that Congress provided any form of government. Though the U.S. Air Force became an independent entity of the DoD on September 18, 1947, its roots trace back to the early 1900s when the Army Signal Corps founded an Aeronautic Division in 1907. In 1915, the U.S. Lifesaving Service combined with the Revenue Cutter Service (Revenue Marine Service) to form the United States Coast Guard. The U.S. Coast Guard recognizes August 4, 1790, as the service birthday (Coast Guard Day) when Congress approved Secretary of the Treasury Alexander Hamilton's proposal to construct ten cutters establishing the Revenue Marine Service. In 1924, when Sitka National Cemetery was designated, most of the interments were soldiers and sailors from the Marine base and Naval hospital. Since then, there have been several acreage modifications: in 1925, a revision of the executive order reduced the acreage from 3.98 acres to 1.19 acres; in 1957, Sheldon Jackson Junior College donated approximately one acre; a donation of 0.20 acres was made in 1959 by the Board of National Missions of the Presbyterian Church of the United States; and the Department of Interior transferred approximately two acres in the mid-1980s. Sitka National Cemetery currently encompasses 4.3 acres. The remote Sitka National Cemetery is located half a mile east of the center of town and is dominated by the natural beauty of the mountains and waters of Sitka Bay. The only access to Sitka is by air, marine highway or weekly ferry from Seattle, WA. In Alaska, the Metlakatla Veterans Cemetery officially opened in July of 2022.
In Oregon, Portland was three separate towns until the first bridges were built in 1887 and 1888. In 1912, Oregon Railway and Navigation Company (ORNC) replaced the first steel train bridge over the Willamette River. Later in 1917, ORNC donated land for the establishment of a Medical School and what would eventually become the Portland VA Medical Center (PVAMC). Portland's first Veterans hospital opened its doors in 1921 and was transferred to the U.S. Veterans Bureau in 1922. The Oregon Journal newspaper reported that the land for the hospital “was donated to the state of Oregon for the University of Oregon medical school by Mrs. C.S. Jackson and Philip L. Jackson as a memorial to the late publisher of The Journal. From the area, 25 acres were donated to the government by the regents of the medical school.” The value of the Marquam Hill at that time was about $2,750 per acre. Initial site preparation was started on February 3, 1927, with construction for the original hospital commencing one year later. The first 13 buildings were completed and activated by December 1928. Dedication of PVAMC was held in 1929.
 PVAMC is situated atop a 450-foot-tall basalt-rock hill south of downtown. PVAMC began partnership with University of Oregon in 1948. After University of Oregon moved south in 1981, the university was renamed Oregon Health & Science University (OHSU). The state of Oregon also donated 102 acres of land for construction of Willamette National Cemetery in Happy Valley. In 1987, the VA expanded PVAMC and built a skybridge with federal funding secured by Senator Mark Hatfield. Once completed, the skybridge allowed direct transportation of patients and supplies over a 150-foot-deep ravine between PVAMC and OHSU. At the time of the dedication in 1992, the 660-foot-long skybridge was the longest suspended pedestrian skybridge in the United States. In 2006, an aeriel tram service began roundtrip operations between the OHSU South Waterfront campus along with the Willamette River to the VA/OHSU campus on Marquam Hill. From the South Waterfront, aeriel tram service arrives at the Peter O. Kohler Pavilion.
PVAMC is situated atop a 450-foot-tall basalt-rock hill south of downtown. PVAMC began partnership with University of Oregon in 1948. After University of Oregon moved south in 1981, the university was renamed Oregon Health & Science University (OHSU). The state of Oregon also donated 102 acres of land for construction of Willamette National Cemetery in Happy Valley. In 1987, the VA expanded PVAMC and built a skybridge with federal funding secured by Senator Mark Hatfield. Once completed, the skybridge allowed direct transportation of patients and supplies over a 150-foot-deep ravine between PVAMC and OHSU. At the time of the dedication in 1992, the 660-foot-long skybridge was the longest suspended pedestrian skybridge in the United States. In 2006, an aeriel tram service began roundtrip operations between the OHSU South Waterfront campus along with the Willamette River to the VA/OHSU campus on Marquam Hill. From the South Waterfront, aeriel tram service arrives at the Peter O. Kohler Pavilion.
Camp Vancouver, the first U.S. Army base of the Pacific Northwest, opened in Washington in 1849. Vancouver Barracks National Cemetery was also established in the mid-1800's. In 1917, an interstate bridge was built connecting Vancouver, Washington and Portland, Oregon. Camp Vancouver was later renamed Columbia Barracks, Fort Vancouver, and Vancouver Barracks. VA Portland Health Care System (VAPORHCS) serves Veterans in Oregon and Southwest Washington with two main divisions: PVAMC and Vancouver VA Medical Center (VVAMC). VAPORHCS CBOCs and Vet Centers are located in Astoria, Bend, Boardman, Brookings, Eugene, Fairview, Grants Pass, Hines, Hillsboro, Klamath Falls, LaGrande, Lincoln City, Newport, Portland, Salem, The Dalles, and West Linn. In Oregon, VA Medical Centers are also located in Roseburg and White City.
The VA has been serving Veterans in Vancouver since May 1946 when President Truman authorized the transfer of the U.S. Army Barnes General Hospital to the Veterans Administration. Established in 1941, Barnes General Hospital of Vancouver Barracks, was named after Major General Joseph K. Barnes, the 12th surgeon general of the U.S. Army. Public Law 79-293 (The Department of Medicine and Surgery Act), signed by President Harry Truman in 1946, drove further modernization and expansion of the VA medical system and partnerships with research universities. Pearson Air Museum, part of Fort Vancouver National Historic Site, narrates the history of Pearson Field, one of the nation's oldest continuously operating airfields. A UH-1 Huey flown by the U.S. Navy Helicopter Attack Squadron Light Three (HAL-3) Seawolves, is exhibited at VVAMC Military Museum. VA's Vancouver Military Museum, situated in a World War II-era building, was once utilized for radio transmissions for Pearson Field. New construction of VVAMC was completed in the 1980s and Vancouver Barracks was closed in 2011. In 2025, VVAMC opened a imaging facility and adding MRI machines, X-ray rooms, ultrasound stations, and a CT scanning machine. In Washington, VA Medical Centers are also located in Seattle, Walla Walla, and Spokane.
 When the U.S. joined World War I in 1917, Congress introduced a range of Veterans benefits including disability compensation, insurance, and vocational rehabilitation. The 1917 War Risk Insurance Act sought to ensure the welfare of service members and their families both for the duration of the conflict and far into the future. The bill allowed military personnel to purchase up to $10,000 in yearly renewable insurance from the government covering them against death or total disability, regardless of cause. These short-term policies could be converted after the war into various types of permanent insurance plans similar to those marketed by commercial companies. Known as the first "total war," World War I saw combatants commit all resources on an unprecedented scale. Being the first fully mechanized war, many soldiers requiring specialized care from exposure to mustard gas and chemicals needed attention post-war. In 1918, Congress gave the Bureau of War Risk Insurance and Public Health Service the job of running hospitals for returning veterans.
When the U.S. joined World War I in 1917, Congress introduced a range of Veterans benefits including disability compensation, insurance, and vocational rehabilitation. The 1917 War Risk Insurance Act sought to ensure the welfare of service members and their families both for the duration of the conflict and far into the future. The bill allowed military personnel to purchase up to $10,000 in yearly renewable insurance from the government covering them against death or total disability, regardless of cause. These short-term policies could be converted after the war into various types of permanent insurance plans similar to those marketed by commercial companies. Known as the first "total war," World War I saw combatants commit all resources on an unprecedented scale. Being the first fully mechanized war, many soldiers requiring specialized care from exposure to mustard gas and chemicals needed attention post-war. In 1918, Congress gave the Bureau of War Risk Insurance and Public Health Service the job of running hospitals for returning veterans.
However, combat stopped seven months earlier when an armistice between the Allied nations and Germany took effect at the eleventh hour of the eleventh day of the eleventh month. Thus, November 11, 1918, is widely considered the end of "the war to end all wars." Veterans Day is still celebrated on November 11 every year, regardless of the weekday. Observing Veterans Day on November 11 maintains the historical importance of the date. The Veterans Day National Ceremony is held each year on November 11th at Arlington National Cemetery. The ceremony commences precisely at 11:00 a.m. with a wreath laying at the Tomb of the Unknowns and continues inside the Memorial Amphitheater with a parade of colors by Veterans’ organizations and remarks from dignitaries. The ceremony is intended to honor and thank all who served in the United States Armed Forces. Veterans Day is always observed officially on November 11, regardless of the day of the week on which it falls.
The Veterans Day National Ceremony, like most ceremonies around the nation, is held on Veterans Day itself. However, when Veterans Day falls on a weekday, many communities choose to hold Veterans Day parades or other celebrations on the weekend before or after November 11 so that more people can participate. The Veterans Day National Committee recognizes select Veterans Day observances throughout the country that represent fitting tributes to America’s heroes and serve as models for other communities to follow in planning their own observances. Each September, posters are distributed to schools, state governments, Veterans Day Regional Sites, the military services, and veterans service organizations. Poster requests are fulfilled until the inventory is exhausted. You can download or print your own poster from the Veterans Day Poster Gallery. Each year the VA and the Veterans Day National Committee provide a Teachers Resource Guide.
 In 1918, Congress assigned two Treasury agencies - the Bureau of War Risk Insurance and the Public Health Service - the responsibility of operating hospitals specifically for returning World War I veterans. After World War I, service members had to navigate the bureaucracies of three different federal agencies to obtain benefits: the U.S. Public Health Service (PHS) for medical and hospital care, the Federal Board for Vocational Education for rehabilitation, education, and job training, and the Bureau of War Risk Insurance (BWRI) for insurance and compensation. In the spring of 1919, Congress also approved the largest federal hospital construction program in U.S. history to date, appropriating more than $9 million for the building of new hospitals and the improvement of existing ones. When Warren G. Harding accepted the Republican nomination for president in 1920, he made a solemn promise to the more than four million Americans who had served in what was then known as the World War: "It is not only a duty, it is a privilege to see that the sacrifices made shall be requited, and that those still suffering from casualties and disabilities shall be abundantly aided and restored to the highest capabilities of citizenship and enjoyment." By June 1920, the PHS reported that it was operating an additional 28 hospitals of three different types: general medical, tuberculosis, and neuropsychiatric. Sixty-five million men and women participated in World War I, and historians estimate that as many as 10 million men died while another 20 million were wounded. Known at the time as "The Great War," World War I officially concluded with the signing of the Treaty of Versailles on June 28, 1919, at the Palace of Versailles near the town of Versailles, France. The World War I Victory Medal was awarded for service between 06 April 1917 and 11 November 1918 or with either of the following expeditions:
In 1918, Congress assigned two Treasury agencies - the Bureau of War Risk Insurance and the Public Health Service - the responsibility of operating hospitals specifically for returning World War I veterans. After World War I, service members had to navigate the bureaucracies of three different federal agencies to obtain benefits: the U.S. Public Health Service (PHS) for medical and hospital care, the Federal Board for Vocational Education for rehabilitation, education, and job training, and the Bureau of War Risk Insurance (BWRI) for insurance and compensation. In the spring of 1919, Congress also approved the largest federal hospital construction program in U.S. history to date, appropriating more than $9 million for the building of new hospitals and the improvement of existing ones. When Warren G. Harding accepted the Republican nomination for president in 1920, he made a solemn promise to the more than four million Americans who had served in what was then known as the World War: "It is not only a duty, it is a privilege to see that the sacrifices made shall be requited, and that those still suffering from casualties and disabilities shall be abundantly aided and restored to the highest capabilities of citizenship and enjoyment." By June 1920, the PHS reported that it was operating an additional 28 hospitals of three different types: general medical, tuberculosis, and neuropsychiatric. Sixty-five million men and women participated in World War I, and historians estimate that as many as 10 million men died while another 20 million were wounded. Known at the time as "The Great War," World War I officially concluded with the signing of the Treaty of Versailles on June 28, 1919, at the Palace of Versailles near the town of Versailles, France. The World War I Victory Medal was awarded for service between 06 April 1917 and 11 November 1918 or with either of the following expeditions:
- American Expeditionary Forces in European Russia, between 12 November 1918 and 05 August 1919.
- American Expeditionary Forces Siberia, between 23 November 1918 and 01 April 1920.
Following World War I, Henry Ford donated 50 Model T Fords to war Veterans in attending the second national convention of the Disabled American Veterans of the World War (DAVWW). Henry Ford initiated the hiring of disabled veterans returning from World War I to work at the company. Later renamed Disabled American Veterans (DAV), the partnership continued to grow and bothFord and DAV continue to lead the nation in Veterans employment. The early 1900's saw continued improvements in transportation systems. In Oregon, the Columbia River Highway Project was the first planned scenic highway project in the United States. Known as "The King of Roads", the Columbia River Highway opened in 1916 and became the first designated scenic highway of the United States. For over a century, Ford Motor Company has maintained a strong relationship with Disabled American Veterans (DAV). DAV currently operates a nationwide fleet of vehicles offering free medical transportation for ill and injured veterans. When the federal government ended its transportation assistance program for veterans attending medical appointments, DAV stepped in to provide the necessary support. To determine if there is a van available nearby, consult the DAV Hospital Service Coordinator Directory and contact your nearest HSC for information or help.
 In 1920, World War I veteran Hamilton Fish Jr. introduced a bill to repatriate the remains of an unidentified American soldier who would symbolize no particular region, belief, or ethnicity from the recent war and embody the essence of America and the ultimate sacrifice of its heroic fallen. By October 1921, one unknown U.S. service member who perished in World War I was randomly selected to represent "the soul of America and the supreme sacrifice of her heroic dead," as stated in the legislation permitting the burial. On November 11, 1921, a ceremony took place at Arlington National Cemetery to bury this service member in a newly established, temporary tomb. During the funeral, President Warren G. Harding awarded the Medal of Honor to the individual's casket.
In 1920, World War I veteran Hamilton Fish Jr. introduced a bill to repatriate the remains of an unidentified American soldier who would symbolize no particular region, belief, or ethnicity from the recent war and embody the essence of America and the ultimate sacrifice of its heroic fallen. By October 1921, one unknown U.S. service member who perished in World War I was randomly selected to represent "the soul of America and the supreme sacrifice of her heroic dead," as stated in the legislation permitting the burial. On November 11, 1921, a ceremony took place at Arlington National Cemetery to bury this service member in a newly established, temporary tomb. During the funeral, President Warren G. Harding awarded the Medal of Honor to the individual's casket.
Land at Fort Walla Walla was transferred to the then U.S. Veterans Bureau for a hospital in 1921. Fort Walla Walla was one of the longest-occupied military posts in the Pacific Northwest dating back to 1856. The Veterans hospital was renamed Jonathan M. Wainwright Memorial VA Medical Center on Veterans Day 1996, in honor of Jonathan M. Wainwright IV, a Walla Walla native son and war hero. Wainwright was born on Fort Walla Walla grounds August 23, 1883; he was a WWII POW in Manchuria, China from 1942 to 1945 and was liberated August 16, 1945, just 6 days before his birthday. A survivor of the Bataan Death March, he was liberated from the POW camp on August 16, 1945. Wainwright received numerous medals, including the Medal of Honor September 10, 1945, which was presented to him by President Truman. The Jonathan M. Wainwright VA serves Veterans spanning 16 counties and 3 states. The Walla Walla Veterans Home is co-located on the campus of the Jonathan M. Wainwright Memorial VA Medical Center.
 In April 1921, a Presidential committee suggested merging the Bureau of War Risk Insurance, Federal Board of Vocational Education, and Public Health Service into an independent federal agency led by an executive reporting directly to the president. Congress adopted this proposal and passed Public Law 67-47, also known as the Sweet Act after its sponsor, creating the Veterans Bureau. Following World War I, Tuberculosis and Neuropsychiatric hospitals were established for Veterans with respiratory or mental health issues. President Harding signed Public Law 67-47 on August 8, 1921, formally establishing the Veterans Bureau by uniting the three World War I Veterans programs. However, not all government services for Veterans were included in the Veterans Bureau; the Pension Bureau, which managed pensions for soldiers and sailors from earlier conflicts within the Department of Interior, remained separate. Similarly, the National Home for Disabled Volunteer Soldiers stayed distinct until they were eventually merged with the Veterans Bureau by executive order in 1930.
In April 1921, a Presidential committee suggested merging the Bureau of War Risk Insurance, Federal Board of Vocational Education, and Public Health Service into an independent federal agency led by an executive reporting directly to the president. Congress adopted this proposal and passed Public Law 67-47, also known as the Sweet Act after its sponsor, creating the Veterans Bureau. Following World War I, Tuberculosis and Neuropsychiatric hospitals were established for Veterans with respiratory or mental health issues. President Harding signed Public Law 67-47 on August 8, 1921, formally establishing the Veterans Bureau by uniting the three World War I Veterans programs. However, not all government services for Veterans were included in the Veterans Bureau; the Pension Bureau, which managed pensions for soldiers and sailors from earlier conflicts within the Department of Interior, remained separate. Similarly, the National Home for Disabled Volunteer Soldiers stayed distinct until they were eventually merged with the Veterans Bureau by executive order in 1930.
 President Harding traveled throughout the Pacific Northwest in 1923, visiting U.S. Veterans Hospital, No. 77, in Portland, Oregon on Independence Day. Pledging aid to the Service Men and the Service Force of the Hospital, President Harding, spoke of the Supreme Tragedy of War, "The great, the supreme tragedy of war is not that it sacrifices so many lives, but that it impairs men for the active service of life. Your big fight is to rise above the impairment. I wish you the best ever, men, and I desire to assure you that if matters are not going right with you, and the government learns of it, it will make an honest effort to try to correct conditions, because in the grateful heart of the Republic is the determination to do the best that can be done to bring you men who offered everything back to a full participation in active life." Along with visiting U.S. Veterans Hospital, No. 77, President Harding visited and spoke with hospitalized Veterans at U.S. Veterans Hospital No. 59 in Tacoma, Washington; U.S. Army Hospital in Denver, Colorado; and U.S. Veterans Hospital in Helena, Montana.
President Harding traveled throughout the Pacific Northwest in 1923, visiting U.S. Veterans Hospital, No. 77, in Portland, Oregon on Independence Day. Pledging aid to the Service Men and the Service Force of the Hospital, President Harding, spoke of the Supreme Tragedy of War, "The great, the supreme tragedy of war is not that it sacrifices so many lives, but that it impairs men for the active service of life. Your big fight is to rise above the impairment. I wish you the best ever, men, and I desire to assure you that if matters are not going right with you, and the government learns of it, it will make an honest effort to try to correct conditions, because in the grateful heart of the Republic is the determination to do the best that can be done to bring you men who offered everything back to a full participation in active life." Along with visiting U.S. Veterans Hospital, No. 77, President Harding visited and spoke with hospitalized Veterans at U.S. Veterans Hospital No. 59 in Tacoma, Washington; U.S. Army Hospital in Denver, Colorado; and U.S. Veterans Hospital in Helena, Montana.
The American Lake VA Medical Center was established in 1923 in Tacoma, Washington, becoming the 94th Veterans Hospital constructed by the War Department to serve World War I Veterans. The Secretary of the Army granted the Veteran Bureau a revocable license to use 377 acres of the 87,000-acre Fort Lewis property in Washington state. On March 15, 1924, the hospital admitted its first 50 patients, transferred from Western State Hospital at Fort Steilacoom to American Lake VA Medical Center. After Fort Steilacoom's closure, the hospital was maintained by Washington Territory under the name Insane Asylum of Washington Territory. Through land acquisitions, auctions, and authorized donations from the U.S. Army, Western State Hospital has continued its operations and is now the sixth-largest psychiatric hospital in the United States. In 1948, American Lake VA saw the construction of VA's first facilities designed for women Veterans. In 1976, Washington state legislature passed new laws creating the Department of Veterans Affairs for Washington State.
Following World War I, General Charles Summerall suggested that Congress reinstate the "Badge of Military Merit." In January 1928, the Army's Office of The Adjutant General was directed to organize the documents related to this proposed medal. Included in these materials was a preliminary sketch of a circular medal with a concave center featuring a raised heart, inscribed on the reverse side with "For Military Merit." On January 7, 1931, Summerall's successor, General Douglas MacArthur, reopened work on a new design. Miss Elizabeth Will, an Army heraldic specialist in the Office of the Quartermaster General, was named to redesign the newly revived medal, which became known as the Purple Heart. On February 22, 1932 -- marking the 200th anniversary of George Washington’s birth -- the War Department (now the Department of Defense) introduced the Purple Heart award in General Order No. 3, "By order of the President of the United States, the Purple Heart established by General George Washington at Newburgh, August 7, 1782, during the War of the Revolution, is hereby revived out of respect to his memory and military achievements".
 U.S. Army General Frank T. Hines, the VA's longest-serving head, recommended the integration and coordination of all Veterans services into a single agency. The stock market crash of 1929 and the ensuing Great Depression resulted in unprecedented unemployment and economic hardships for Americans. Within a week, the stock market plummeted by nearly half of its record highs, leading to billions of dollars in losses and financial ruin for thousands of investors. In addition to the challenging times of the Great Depression, General Hines steered the Veterans Bureau and Veterans Administration through the largest federal hospital construction program, opening of benefits to Native Americans and women, and the G.I. Bill’s first year of implementation. By 1929, the National Homes had expanded to 11 institutions across the country.
U.S. Army General Frank T. Hines, the VA's longest-serving head, recommended the integration and coordination of all Veterans services into a single agency. The stock market crash of 1929 and the ensuing Great Depression resulted in unprecedented unemployment and economic hardships for Americans. Within a week, the stock market plummeted by nearly half of its record highs, leading to billions of dollars in losses and financial ruin for thousands of investors. In addition to the challenging times of the Great Depression, General Hines steered the Veterans Bureau and Veterans Administration through the largest federal hospital construction program, opening of benefits to Native Americans and women, and the G.I. Bill’s first year of implementation. By 1929, the National Homes had expanded to 11 institutions across the country.
Despite these trying circumstances, President Herbert Hoover sought to merge three agencies administering Veterans benefits into the Veterans Administration. In his State of the Union address on December 3, 1929, President Hoover apprised Congress, "The administration of all laws concerning the veterans and their dependents has been upon the basis of dealing generously, humanely, and justly… I am convinced that we will gain in efficiency, economy, and more uniform administration and better definition of national policies if the Pension Bureau, the National Home for Volunteer Soldiers, and the Veterans’ Bureau are brought together under a single agency."
 Congress empowered the president to “consolidate and coordinate Government activities affecting war Veterans.” A bill supporting the President’s initiative passed through Congress and was signed into law by President Hoover on July 3, 1930. The major consolidation took place on July 21, 1930, when President Hoover merged the Veterans Bureau with the National Home for Disabled Volunteer Soldiers and the Pension Bureau, rebranding it as the Veterans Administration. Executive Order 5398 abolished the National Home for Disabled Volunteer Soldiers and its Board of Managers; at that time the National Home branches were reorganized as the Bureau of National Homes within the VA. After the VA was established, the National Homes were converted to domiciliary care in September to provide services to economically disadvantaged Veterans. The VA's transition from permanent homes to short term medical care is reflected in the architectural changes at National Home branches. After the creation of the Veteran's Administration, building and campus design became more standardized. Over the years, the VA has continued to improve facilities to serve the changing needs of veterans; however, the unique campuses and architecture of the original National Home branches remain, providing insight for visitors as to how the Federal Government cared for and continues to provide for veterans. General Hines led the newly formed VA until 1945.
Congress empowered the president to “consolidate and coordinate Government activities affecting war Veterans.” A bill supporting the President’s initiative passed through Congress and was signed into law by President Hoover on July 3, 1930. The major consolidation took place on July 21, 1930, when President Hoover merged the Veterans Bureau with the National Home for Disabled Volunteer Soldiers and the Pension Bureau, rebranding it as the Veterans Administration. Executive Order 5398 abolished the National Home for Disabled Volunteer Soldiers and its Board of Managers; at that time the National Home branches were reorganized as the Bureau of National Homes within the VA. After the VA was established, the National Homes were converted to domiciliary care in September to provide services to economically disadvantaged Veterans. The VA's transition from permanent homes to short term medical care is reflected in the architectural changes at National Home branches. After the creation of the Veteran's Administration, building and campus design became more standardized. Over the years, the VA has continued to improve facilities to serve the changing needs of veterans; however, the unique campuses and architecture of the original National Home branches remain, providing insight for visitors as to how the Federal Government cared for and continues to provide for veterans. General Hines led the newly formed VA until 1945.
The location of Roseburg VA Medical Center in Oregon was originally a 2nd generation NHDVS dating back 1893. A new VA Medical Center was built in 1933. VA took charge of the Roseburg National Cemetery the following year. The new construction added a bridge to connect the main campus over the South Umpqua River. Within a few years later, nearly 700 neuropsychiatry beds were added. Then again in the 1970's, hundreds of more beds were added to expand domiciliary care. Roseburg VA Medical Center expanded again in 1994 with ambulatory care and a new outpatient clinic. In 2023, the Roseburg VA Medical Center opened a 17-bed hospice care facility. Roseburg VA Medical Center provides Veterans with health care services in Douglas, Lane, Coos, and Curry counties in Oregon. Fort Lawton in Seattle, Washington built in 1896 was named after Maj. Gen. Henry Ware Lawton. Lawton, OK, home of U.S. Army Fort Sill is also named after Maj. Gen. Lawton. Fort Lawton Post Cemetery opened several years later. Construction of the Fort Worden military defense installation began in 1896. Fort Worden Post Cemetery was authorized in 1903 as the official burial grounds for the three Puget Sound harbor defense forts; Fort Casey, Fort Flagler, and Fort Worden.
 In 1936, Congress designated the last Sunday in September as Gold Star Mother’s Day, which is now celebrated as Gold Star Mother’s and Family’s Day. During World War II, many families displayed a banner with a blue star for each family member serving in the armed forces and a gold star for any member who had paid the supreme sacrifice in the war. Accordingly, the term “gold star mother” referred to any woman who had lost a child in defense of the country. America’s first peacetime draft was instituted with the Selective Training and Service Act of 1940, which required men between the ages of 21 and 34 to train and serve with the Army for 1 year, after which the men could go home while remaining in the Army’s reserve component for 10 years. The Act also established the Selective Service System as an independent federal agency. On October 16, 1940, the date selected for registration, more than 16 million men registered, and between November 1940 and October 1946, over 10 million men entered military service through the Selective Service System. Despite the disappointing aftermath, the War Risk insurance program introduced in 1917 was considered enough of a success for Congress to authorize a new version, called National Service Life Insurance, on the eve of World War II. After a slow start, almost all of the more than 16 million Americans who served in the war would enroll in this insurance program. World War II was the most extensive conflict in history, involving over 100 million individuals in military service.
In 1936, Congress designated the last Sunday in September as Gold Star Mother’s Day, which is now celebrated as Gold Star Mother’s and Family’s Day. During World War II, many families displayed a banner with a blue star for each family member serving in the armed forces and a gold star for any member who had paid the supreme sacrifice in the war. Accordingly, the term “gold star mother” referred to any woman who had lost a child in defense of the country. America’s first peacetime draft was instituted with the Selective Training and Service Act of 1940, which required men between the ages of 21 and 34 to train and serve with the Army for 1 year, after which the men could go home while remaining in the Army’s reserve component for 10 years. The Act also established the Selective Service System as an independent federal agency. On October 16, 1940, the date selected for registration, more than 16 million men registered, and between November 1940 and October 1946, over 10 million men entered military service through the Selective Service System. Despite the disappointing aftermath, the War Risk insurance program introduced in 1917 was considered enough of a success for Congress to authorize a new version, called National Service Life Insurance, on the eve of World War II. After a slow start, almost all of the more than 16 million Americans who served in the war would enroll in this insurance program. World War II was the most extensive conflict in history, involving over 100 million individuals in military service.
 After the attack on Pearl Harbor, the Selective Training and Service Act of 1940 original expiration date of May 15, 1945, was extended to the duration of the war plus 6 months. In June of 1942, Oregon's Fort Stevens was attacked by a Japanese submarine. On December 5th, 1942, the U.S. Navy, Marine Corps, and Coast Guard were given authorization to issue Purple Hearts, retroactive to the Pearl Harbor attack that killed thousands of Navy personnel and led the United States into World War II. The Presidential Executive Order of 1942 specified that the Purple Heart would be awarded to individuals "wounded in action against an enemy of the United States, or as a result of an act of such enemy, provided such wounds necessitate treatment by a medical officer." Since 1999, Purple Heart recipients have been assigned to VA’s enrollment Priority Group 3 unless eligible for higher groups (1 or 2) based on service-connected disabilities. The VA reimburses verified Purple Heart recipients for any medical care copays paid to the VA on or after November 30, 1999—the date the Purple Heart Benefit was enacted—or the date the Purple Heart was awarded, whichever is later. Over 1 million Purple Hearts were issued during World War II. John F. Kennedy is the only U.S. President to have received the Purple Heart.
After the attack on Pearl Harbor, the Selective Training and Service Act of 1940 original expiration date of May 15, 1945, was extended to the duration of the war plus 6 months. In June of 1942, Oregon's Fort Stevens was attacked by a Japanese submarine. On December 5th, 1942, the U.S. Navy, Marine Corps, and Coast Guard were given authorization to issue Purple Hearts, retroactive to the Pearl Harbor attack that killed thousands of Navy personnel and led the United States into World War II. The Presidential Executive Order of 1942 specified that the Purple Heart would be awarded to individuals "wounded in action against an enemy of the United States, or as a result of an act of such enemy, provided such wounds necessitate treatment by a medical officer." Since 1999, Purple Heart recipients have been assigned to VA’s enrollment Priority Group 3 unless eligible for higher groups (1 or 2) based on service-connected disabilities. The VA reimburses verified Purple Heart recipients for any medical care copays paid to the VA on or after November 30, 1999—the date the Purple Heart Benefit was enacted—or the date the Purple Heart was awarded, whichever is later. Over 1 million Purple Hearts were issued during World War II. John F. Kennedy is the only U.S. President to have received the Purple Heart.
In 1942, the War Department undertook a significant construction project, erecting over 1,000 buildings in the Agate Desert near Medford, Oregon. Officially dedicated on September 15, 1942, U.S. Army Camp White became a training installation for World War II military personnel. The camp was named after Major General George A. White, who served as the adjutant general of the Oregon National Guard (ONG) for nearly 27 years. After World War II, the hospital buildings of Camp White began operation as White City VA Medical Center Domiciliary. Eagle Point National Cemetery opened at White City VA Domiciliary in 1952. White City VA facilities feature 255 residential rehabilitation beds and provides primary and mental health care through its outpatient department. Major General White was one of the founding members of the American Legion Veterans Service Organization (VSO). In 2018, the ONG inaugurated the new Maj. Gen. George A. White Headquarters. White City VA Medical Center functions as a teaching hospital offering a full range of services, supported by state-of-the-art technology, education, and research.  In 1943, the U.S. Navy opened Naval Air Station Klamath Falls in Oregon. That same year, the 142nd wing of the U.S. Air Force was stood up in Portland. Two years later, 29 Veterans hospitals were announced for construction across the United States. In the Pacific Northwest, this included hospitals in Klamath Falls, Oregon and Spokane, Washington. Klamath Falls continues to serve Veterans with a VA CBOC providing primary care to help Veterans stay healthy and well. The VA's Southern Oregon Healthcare System serves Veterans in Jackson, Josephine, Klamath, and Lake counties in Oregon, as well as Siskiyou and Del Norte counties in northern California. The VA Southern Oregon Rehabilitation Center & Clinics (VA SORCC) in White City provides training programs for students at the college, university, and postgraduate levels. Klamath Falls is currently home to the 173rd Fighter Wing of the U.S. Air Force, Oregon Air National Guard.
In 1943, the U.S. Navy opened Naval Air Station Klamath Falls in Oregon. That same year, the 142nd wing of the U.S. Air Force was stood up in Portland. Two years later, 29 Veterans hospitals were announced for construction across the United States. In the Pacific Northwest, this included hospitals in Klamath Falls, Oregon and Spokane, Washington. Klamath Falls continues to serve Veterans with a VA CBOC providing primary care to help Veterans stay healthy and well. The VA's Southern Oregon Healthcare System serves Veterans in Jackson, Josephine, Klamath, and Lake counties in Oregon, as well as Siskiyou and Del Norte counties in northern California. The VA Southern Oregon Rehabilitation Center & Clinics (VA SORCC) in White City provides training programs for students at the college, university, and postgraduate levels. Klamath Falls is currently home to the 173rd Fighter Wing of the U.S. Air Force, Oregon Air National Guard.
The city of Spokane and the county donated over 200 acres of land for the new VA expansion. In less than a year, a 1,500-bed hospital was built to care for the wounded returning from war. New construction of a Veterans hospital in Spokane Washington began in 1950. In 2013, Spokane VA Medical Center was renamed Mann-Grandstaff VA Medical Center in honor of Medal of Honor recipients; Private First-Class Joe Eugene Mann and Platoon Sergeant Bruce Alan Grandstaff. PFC Mann of Reardon died in combat during WWII. Platoon SGT Grandstaff of Spokane died in combat during Vietnam. In addition to the VA Medical Center in Spokane, VA's Spokane Healthcare System serves Veterans with clinics in eastern Washington, northern Idaho, and northwestern Montana. The Spokane Veterans Home is operated and maintained by Washington State. Tertiary care referrals at Mann-Grandstaff VA Medical Center are coordinated with VAPORHCS and to VA Puget Sound Healthcare System (VAPSHCS). Spokane's support of Veterans followed the business and public-minded citizens who had already purchased 1,400 acres for what would become Fairchild Air Force Base. Washington State Veterans Cemetery – Medical Lake was dedicated May 31, 2010, and opened for interments on Jun 7, 2010.
 Construction of the Seattle VA Medical Center started in the 1940s, utilizing a 44-acre nine-hole golf course donated by Seattle at Jefferson Park, which had been the U.S. Army's largest recreation center during World War II. The Seattle VA Medical Center was officially dedicated on May 15, 1951. That same year, VAPSHCS began its collaboration with the University of Washington (UW) School of Medicine. UW is the largest psychiatry residency program in the United States training psychiatrists, psychologists and medical students across five states in Washington, Alaska, Idaho, Montana, and Wyoming. Significant expansions of research and medical care facilities occurred in 1967 and 1985. On Veterans Day 1993, Tahoma National Cemetery was established in Kent, Washington and dedicated in the fall of 1997. VAPSHCS serves Veterans from a five-state area in the Pacific Northwest with two main divisions: American Lake VA Medical Center and Seattle VA Medical Center. VA Medical Centers are also located in Spokane, Vancouver, and Walla Walla. VA CBOCs and Vet Centers are located in Bellingham, Bellevue, Bremerton, Edmunds, Everett, Federal Way, Lacey, Mount Vernon, Olympia, Port Angeles, Puyallup, Richland, Renton, Silverdale, Seattle, Spokane, Union Gap, Vancouver, Walla Walla, Wenatchee, and Yakima.
Construction of the Seattle VA Medical Center started in the 1940s, utilizing a 44-acre nine-hole golf course donated by Seattle at Jefferson Park, which had been the U.S. Army's largest recreation center during World War II. The Seattle VA Medical Center was officially dedicated on May 15, 1951. That same year, VAPSHCS began its collaboration with the University of Washington (UW) School of Medicine. UW is the largest psychiatry residency program in the United States training psychiatrists, psychologists and medical students across five states in Washington, Alaska, Idaho, Montana, and Wyoming. Significant expansions of research and medical care facilities occurred in 1967 and 1985. On Veterans Day 1993, Tahoma National Cemetery was established in Kent, Washington and dedicated in the fall of 1997. VAPSHCS serves Veterans from a five-state area in the Pacific Northwest with two main divisions: American Lake VA Medical Center and Seattle VA Medical Center. VA Medical Centers are also located in Spokane, Vancouver, and Walla Walla. VA CBOCs and Vet Centers are located in Bellingham, Bellevue, Bremerton, Edmunds, Everett, Federal Way, Lacey, Mount Vernon, Olympia, Port Angeles, Puyallup, Richland, Renton, Silverdale, Seattle, Spokane, Union Gap, Vancouver, Walla Walla, Wenatchee, and Yakima.
On August 14, 1945, Japan surrendered, ending the war in the Pacific. Americans everywhere celebrated the arrival of “V-J Day.” People were particularly relieved that the surrender removed the need for a costly invasion of Japan in terms of human lives and property. From New York to San Francisco, crowds filled the streets to express gratitude and celebrate the victory of freedom. General Omar Bradley announced that VA would construct 183 new hospitals—105 general, 49 neuropsychiatric, and 29 for tuberculosis—adding 151,500 beds across 39 states. The first female doctors were hired, and VA Memorandum No. 2 of 1946 established partnerships with medical schools to train physicians and other medical personnel for VA hospitals. During World War II, 39 acres of Fort Richardson were set aside for use as a temporary burial site where deceased soldiers—regardless of nationality—could be laid to rest. Under the international program for the return of war dead, most of the soldiers interred at Fort Richardson were returned to their families. There were, however, some soldiers who remained buried at Fort Richardson either because the next of kin could not be found or their families requested that they remain interred in Alaska. In December 1946, the temporary cemetery at Fort Richardson was made a permanent site, Fort Richardson National Cemetery. In 2010, Fort Richardson merged with Joint Base Elmendorf-Richardson.
 Approximately 16 million Americans participated in WWII, with many now benefiting from VA programs such as Pension and Health Care. The GI Bill, a pioneering piece of legislation, offered Veterans opportunities for education and training; loans for homes, farms, and businesses; unemployment compensation for up to a year; and job placement assistance. Introduced in 1944, the home loan guaranty program aimed to mitigate the severe economic and social disruptions caused by wars. Its primary objectives were to reduce the post-war adjustment challenges faced by millions of service members. During the subsequent economic boom, Veterans leveraged their VA Home Loan benefits to start families and purchase homes. Similar benefits have been extended to Veterans of subsequent conflicts, including the Korean, Vietnam, Operation Desert Shield/Desert Storm (the war in the Persian Gulf). Since its inception in 1944, the GI Bill has enabled eligible Veterans and their family members to obtain financial support for educational or training costs. As a significant innovation, it formed a crucial component of the original Servicemen's Readjustment Act of 1944, Public Law 78-346. Title III of this Act laid down the initial legal framework. The original GI Bill included provisions for education and training, rehabilitation and job placement, zero-down payment home loans, and an expansion that more than doubled the number of VA healthcare facilities for Veterans.
Approximately 16 million Americans participated in WWII, with many now benefiting from VA programs such as Pension and Health Care. The GI Bill, a pioneering piece of legislation, offered Veterans opportunities for education and training; loans for homes, farms, and businesses; unemployment compensation for up to a year; and job placement assistance. Introduced in 1944, the home loan guaranty program aimed to mitigate the severe economic and social disruptions caused by wars. Its primary objectives were to reduce the post-war adjustment challenges faced by millions of service members. During the subsequent economic boom, Veterans leveraged their VA Home Loan benefits to start families and purchase homes. Similar benefits have been extended to Veterans of subsequent conflicts, including the Korean, Vietnam, Operation Desert Shield/Desert Storm (the war in the Persian Gulf). Since its inception in 1944, the GI Bill has enabled eligible Veterans and their family members to obtain financial support for educational or training costs. As a significant innovation, it formed a crucial component of the original Servicemen's Readjustment Act of 1944, Public Law 78-346. Title III of this Act laid down the initial legal framework. The original GI Bill included provisions for education and training, rehabilitation and job placement, zero-down payment home loans, and an expansion that more than doubled the number of VA healthcare facilities for Veterans.
The first Veterans store providing goods and services a part of NHDVS in Dayton, Ohio. The success in Ohio paved the way for Veterans stores to open at other NHDVS branches. Veterans commissaries served as a source of employment. Canteens and stores at VA hospitals expanded into the twentieth century. In August of 1946, the Department of Medicine and Surgery was created alongside the Veterans Administration Voluntary Services (VAVS) and Veterans Canteen Service (VCS). With the establishment of VCS, for the first time, all VA hospitals featured stores and services to benefit Veterans. VCS was created to provide articles of merchandise and services at reasonable prices to Veterans enrolled in VA's healthcare system, caregivers, and visitors. By 1959, 171 canteens were in operation.
Since its conception, VCS' mission continues, incorporating a strategic Veteran-centric approach that emphasizes the importance of service to Veterans and supporting VA's overall mission. VCS has also evolved over the decades, with full-service retail stores, cafeterias, and food courts replacing the gift shops and snack bars that were once the stock in trade of these concessions. The service has branched out in other ways, adding, for instance, an online presence allowing Veterans in rural locations to purchase canteen goods and services. General Omar Bradley's reorganization of VA hospitals added commissaries as part of his larger reform plans to Veterans’ health care. By the time Bradley left VA in 1947, there were 125 VA hospitals. While hospital canteens have changed and expanded to meet the needs of Veterans today, the VCS mission and passion to serve Veterans remains the same decades later.
 VCS proudly offers exclusive online shopping benefits to Veterans enrolled in VA healthcare, their families, and VA employees. Operating as a self-sustaining entity, VCS provides goods and services to Veterans enrolled in VA's Health Care System, their families, caregivers, VA employees, volunteers, and visitors. VCS operates over 200 PatriotStores in VA Medical Centers nationwide. Many VCS stores have updated and expanded to provide customers with a modern, clean and comfortable shopping experience. VCS stores welcomes customers with wider aisles, wood-like floors, enhanced lighting and directional signage. PatriotStores have expanded hours of operation to provide service for customers on weekends at most locations. VCS sponsors five of VA’s National Rehabilitation Events: Golden Age Games, Wheelchair Games, Golf Clinic, Summer Sports Clinic, and Creative Arts Festival. These programs allow disabled Veterans of all ages and abilities to participate in adaptive sports programs and special events. VCS provides monetary donations, sends a support team to each event, and gives away gift bags to Veteran participants. VCS proudly supports these events as they promote wellness, rehabilitation, and camaraderie among the Veteran athletes. The revenues generated by VCS also support various Veteran programs such as Fisher House, Suicide Prevention, disaster relief initiatives, Substance Abuse Cessation, Women Veterans initiatives, Homeless Veterans programs, community stand downs, Welcome Home Celebrations, and more. VCS provides VA Fisher Houses nationwide an offering of coupons to first-time visiting families and serving as their purchasing source for supplies and necessities.
VCS proudly offers exclusive online shopping benefits to Veterans enrolled in VA healthcare, their families, and VA employees. Operating as a self-sustaining entity, VCS provides goods and services to Veterans enrolled in VA's Health Care System, their families, caregivers, VA employees, volunteers, and visitors. VCS operates over 200 PatriotStores in VA Medical Centers nationwide. Many VCS stores have updated and expanded to provide customers with a modern, clean and comfortable shopping experience. VCS stores welcomes customers with wider aisles, wood-like floors, enhanced lighting and directional signage. PatriotStores have expanded hours of operation to provide service for customers on weekends at most locations. VCS sponsors five of VA’s National Rehabilitation Events: Golden Age Games, Wheelchair Games, Golf Clinic, Summer Sports Clinic, and Creative Arts Festival. These programs allow disabled Veterans of all ages and abilities to participate in adaptive sports programs and special events. VCS provides monetary donations, sends a support team to each event, and gives away gift bags to Veteran participants. VCS proudly supports these events as they promote wellness, rehabilitation, and camaraderie among the Veteran athletes. The revenues generated by VCS also support various Veteran programs such as Fisher House, Suicide Prevention, disaster relief initiatives, Substance Abuse Cessation, Women Veterans initiatives, Homeless Veterans programs, community stand downs, Welcome Home Celebrations, and more. VCS provides VA Fisher Houses nationwide an offering of coupons to first-time visiting families and serving as their purchasing source for supplies and necessities.
 President Harry S. Truman signed Executive Order 9981, which mandated the desegregation of the Armed Forces, on July 26, 1948. President Truman led the effort to establish a single holiday for citizens to come together and thank our military members for their patriotic service in support of our country. On August 31, 1949, Secretary of Defense Louis Johnson announced the creation of an Armed Forces Day to replace separate Army, Navy, Marine Corps and Air Force Days. The single day celebration stemmed from the unification of the Armed Forces under the Department of Defense. Through Executive Order 10409 of November 12, 1952, President Truman, retroactively extended Navy, Marine Corps, and Coast Guard eligibility for the Purple Heart back to April 5, 1917, to cover World War I. In 1953, President Dwight D. Eisenhower appointed Harvey V. Higley as head of the Veterans Administration. Segregation at VA Hospitals ended in September 1953 when Higley assumed the role of Administrator of VA. On February 4, 1954, the color designation was removed from all future VA hospitals and outpatient application forms.
President Harry S. Truman signed Executive Order 9981, which mandated the desegregation of the Armed Forces, on July 26, 1948. President Truman led the effort to establish a single holiday for citizens to come together and thank our military members for their patriotic service in support of our country. On August 31, 1949, Secretary of Defense Louis Johnson announced the creation of an Armed Forces Day to replace separate Army, Navy, Marine Corps and Air Force Days. The single day celebration stemmed from the unification of the Armed Forces under the Department of Defense. Through Executive Order 10409 of November 12, 1952, President Truman, retroactively extended Navy, Marine Corps, and Coast Guard eligibility for the Purple Heart back to April 5, 1917, to cover World War I. In 1953, President Dwight D. Eisenhower appointed Harvey V. Higley as head of the Veterans Administration. Segregation at VA Hospitals ended in September 1953 when Higley assumed the role of Administrator of VA. On February 4, 1954, the color designation was removed from all future VA hospitals and outpatient application forms.
The VA's Department of Medicine and Surgery, which was established in the 1940's and was later renamed the Veterans Health Services and Research Administration. The treatment and prevention of mental illness have always been crucial during and after wartime. During World War II, up to one-third of disabling casualties were neuropsychiatric. Before World War II, asylums were typically located in rural areas, intended mainly for custodial care but occasionally for rehabilitation. These facilities were inadequate for dealing with the issues emerging from World War II. During the VA's expansion phase, psychiatry and psychology received less academic and resource support compared to medicine and surgery. Most neuropsychiatric hospitals remained unaffiliated, although some merged with tertiary care institutions. Despite combat stress reactions (CSRs) being documented for over 2,000 years, unscientific principles dictated psychiatry and psychology in the 1940s and 1950s, hindering their progress in light of rapid biomedical advances. Previously, CSRs were known by various names such as Shellshock, Battle Fatigue, Soldier's Heart, and Combat Neurosis.
 The Korean War started prior to the end of World War II. The Korean War - the first major armed clash between Free World and Communist forces - turned the so-called “Cold War” hot, with a divided country’s fight over its borders eventually engaging world powers. The 5.7 million American men and women who served during this conflict each carry their own memories, whether they were on the battlefield, in the air, or supporting those at risk. Of the 1.8 million Americans deployed to Korea, 36,576 lost their lives there, and nearly 7,500 are still unaccounted for from the war. On July 27, 1953, U.S., North Korean, and Chinese military leaders signed the Korean Armistice Agreement.
The Korean War started prior to the end of World War II. The Korean War - the first major armed clash between Free World and Communist forces - turned the so-called “Cold War” hot, with a divided country’s fight over its borders eventually engaging world powers. The 5.7 million American men and women who served during this conflict each carry their own memories, whether they were on the battlefield, in the air, or supporting those at risk. Of the 1.8 million Americans deployed to Korea, 36,576 lost their lives there, and nearly 7,500 are still unaccounted for from the war. On July 27, 1953, U.S., North Korean, and Chinese military leaders signed the Korean Armistice Agreement.
Though the Korean war lasted just over three years, almost 60 years after the conflict ended, American service members continued to maintain peace along the 38th Parallel, the boundary dividing North and South Korea. Even today, a formal peace treaty has not been signed by North and South Korea. Many Korean War veterans have considered themselves overlooked and underappreciated, their place in history sandwiched between World War II and the Vietnam War. The Korean War Veterans Memorial on the National Mall and the commemorative events of the war’s 50th anniversary have provided well-deserved and long-overdue recognition for those who answered their country’s call. However, despite its significance in world history and the sacrifices of those who fought the battles, it is often called “America’s forgotten war.”
 The American Lake Veterans Golf Course, spanning 377 acres, was established in 1955 following World War II. The course was designed as a nine-hole place of respite on the VA hospital near Joint Base Lewis-McChord. After falling into disrepair, the course faced potential abandonment. In 1995, funding for the operation and maintenance of all VA golf courses was eliminated. Nevertheless, American Lake Golf Course continued to operate through a volunteer program. In 2014, Jack Nicklaus designed the new back nine holes and concurrently redesigned the existing front nine holes. Nicklaus’ work is the centerpiece of the $4.5 million project at American Lake called “A Course in Courage: Healing America’s Veterans through Golf.” The renovated front nine reopened in 2022, making it an 18-hole Jack Nicklaus-designed golf course.
The American Lake Veterans Golf Course, spanning 377 acres, was established in 1955 following World War II. The course was designed as a nine-hole place of respite on the VA hospital near Joint Base Lewis-McChord. After falling into disrepair, the course faced potential abandonment. In 1995, funding for the operation and maintenance of all VA golf courses was eliminated. Nevertheless, American Lake Golf Course continued to operate through a volunteer program. In 2014, Jack Nicklaus designed the new back nine holes and concurrently redesigned the existing front nine holes. Nicklaus’ work is the centerpiece of the $4.5 million project at American Lake called “A Course in Courage: Healing America’s Veterans through Golf.” The renovated front nine reopened in 2022, making it an 18-hole Jack Nicklaus-designed golf course.
The American Lake Veterans Golf Course offers rehabilitation, therapy, socialization and support to those who have given so much for our country. American Lake Veterans Golf Course is open to all Veterans, their families and guests. This includes Active-Duty, retired military, National Guard, and reservists of the U.S. Armed Forces. The only non-Veterans allowed to play are employees of VA. Three guests are allowed for each authorized player and must be accompanied by their sponsor while on the course. The American Lake Veterans Golf Course is recognized as the 400th Jack Nicklaus Signature Course. With an unparalleled record of producing the most championship golf courses, Nicklaus Design is synonymous with world-class course design. Notably, Jack Nicklaus is the first athlete and only the fourth individual ever to receive the Presidential Medal of Freedom, the Congressional Gold Medal, and the Lincoln Medal.
The Vietnam War commenced before the conclusion of the Korean War. Official U.S. military involvement in the Vietnam conflict began on August 5, 1964; however, the first American casualty in Vietnam occurred on July 8, 1959. Roughly 2.7 million American men and women served in Vietnam. The U.S. military draft continued, with modifications, during times of peace and conflict until 1973, when the United States converted to an all-voluntary military. During the war, over 58,000 U.S. military personnel lost their lives, and 153,000 sustained injuries. The Veterans’ Administration adapted to meet the needs of Veterans from the Cold War and the transition to an All-Volunteer Force in 1973. The Vietnam war officially ended with a Presidential Proclamation on May 7, 1975. In 1978, the VA started offering special access to medical care, including physical exams, to Vietnam Veterans concerned about Agent Orange exposure. The Agent Orange Act of 1991 codified actions of the Secretary of VA in providing service-connected compensation related to the Vietnam experience and herbacide exposure. This established new procedures for determining whether particular diseases were related to exposure to Agent Orange and other herbacides used in Vietnam. The Vietnam War had a lasting impact, leaving many veterans with untreated Post-Traumatic Stress (PTS), substance abuse issues, and increased physical and mental health problems.
 The Veterans Health Care Amendments Act was passed by Congress in 1979, leading to the establishment of a network of Vet Centers across the country. Vet Centers are community-based counseling centers that provide services to eligible Veterans and active-duty members of the U.S. Armed Forces, including the Army, Navy, Marine Corps, Coast Guard, Air Force, Space Force, National Guard, and Reserve components, as well as their families. Vet Center counselors and outreach staff, many of whom are veterans themselves, are well-equipped to offer confidential counseling, outreach, and referral services, including professional readjustment counseling. The sacrifices made by the over 2 million American men and women who served in Vietnam will always be remembered. Their commitment to duty and selfless service ensured the freedoms and liberties future Americans continue to enjoy. In 1980, the American Psychiatric Association included Post-traumatic Stress Disorder (PTSD) in the Diagnostic and Statistical Manual of Mental Disorders (DSM) based on research involving returning Vietnam War veterans. PTSD is a complex neurobiological condition characterized by physiological, biochemical, and anatomical changes, contributing to excess morbidity and mortality. Vet Centers provide various counseling services and treatment for PTSD.
The Veterans Health Care Amendments Act was passed by Congress in 1979, leading to the establishment of a network of Vet Centers across the country. Vet Centers are community-based counseling centers that provide services to eligible Veterans and active-duty members of the U.S. Armed Forces, including the Army, Navy, Marine Corps, Coast Guard, Air Force, Space Force, National Guard, and Reserve components, as well as their families. Vet Center counselors and outreach staff, many of whom are veterans themselves, are well-equipped to offer confidential counseling, outreach, and referral services, including professional readjustment counseling. The sacrifices made by the over 2 million American men and women who served in Vietnam will always be remembered. Their commitment to duty and selfless service ensured the freedoms and liberties future Americans continue to enjoy. In 1980, the American Psychiatric Association included Post-traumatic Stress Disorder (PTSD) in the Diagnostic and Statistical Manual of Mental Disorders (DSM) based on research involving returning Vietnam War veterans. PTSD is a complex neurobiological condition characterized by physiological, biochemical, and anatomical changes, contributing to excess morbidity and mortality. Vet Centers provide various counseling services and treatment for PTSD.
Family members of service members who died while on active-duty can receive bereavement services at Vet Centers. The 24/7 Vet Center Call Center, reachable at 1-877-WAR-VETS, supports Veterans, service members, and their families in discussing military experiences or challenges faced during the transition after military service or trauma and connects them to the nearest Vet Center. Eligibility for Vet Center services extends to Veterans and current service members, including National Guard and Reserve members, with active military duty in any combat theater or hostile area, such as World War II (including American Merchant Marines), the Korean War, the Vietnam War, Lebanon, Grenada, Desert Storm, Desert Shield, Bosnia, Kosovo, operations in the former Yugoslavia area, Global War on Terrorism, Operation Enduring Freedom (OEF), Operation Freedom's Sentinel, Operation Iraqi Freedom (OIF), and Operation New Dawn (OND).
 On February 23, 1984, President Reagan extended the Purple Heart to include victims of international terrorist attacks. Just before Veterans Day in 1987, President Reagan made a surprise announcement to veterans' organization leaders and members of the Congressional Veterans Affairs Committees, whom he had gathered in the Cabinet Room. He stated his support for legislation that would elevate the Veterans Administration to a cabinet-level department. Highlighting that the veteran population had grown sixfold since VA's founding in 1930, President Reagan remarked, "Veterans have always had a strong voice in our government. It's time to give them the recognition they so rightly deserve." On October 25, 1988, President Reagan signed Public Law 100-527, known as the Department of Veterans Affairs Act, officially making the Veterans Administration the 15th cabinet-level department in the federal government. Established in Article II, Section 2 of the Constitution, the Cabinet’s role is to advise the President on any subject he may require relating to the duties of each member’s respective office. The historic signing ceremony took place at Roosevelt Hall at the National Defense University in Washington, D.C., roughly a week prior to the 1988 presidential election.
On February 23, 1984, President Reagan extended the Purple Heart to include victims of international terrorist attacks. Just before Veterans Day in 1987, President Reagan made a surprise announcement to veterans' organization leaders and members of the Congressional Veterans Affairs Committees, whom he had gathered in the Cabinet Room. He stated his support for legislation that would elevate the Veterans Administration to a cabinet-level department. Highlighting that the veteran population had grown sixfold since VA's founding in 1930, President Reagan remarked, "Veterans have always had a strong voice in our government. It's time to give them the recognition they so rightly deserve." On October 25, 1988, President Reagan signed Public Law 100-527, known as the Department of Veterans Affairs Act, officially making the Veterans Administration the 15th cabinet-level department in the federal government. Established in Article II, Section 2 of the Constitution, the Cabinet’s role is to advise the President on any subject he may require relating to the duties of each member’s respective office. The historic signing ceremony took place at Roosevelt Hall at the National Defense University in Washington, D.C., roughly a week prior to the 1988 presidential election.
Before signing the bill elevating the Veteran’s Administration to Cabinet rank, President Reagan stated, "This bill gives those who have borne America’s battles, who have defended the borders of freedom, who have protected our nation’s security in war and peace—it gives them what they have deserved for so long, a seat at the table in our national affairs. I've said before that America's debt to those who would fight for her defense doesn't end the day the uniform comes off. For the security of our nation, it must not end. Every time a man or woman enlists in the Army, Navy, Air Force, Marines, or Coast Guard, he or she is ready to lay down his or her life for our nation. We must be ready to show that America appreciates what that means. I like to think that this bill gives Cabinet rank not just to an agency within the Government but to every single veteran. And so, in signing this bill, I'm saying to all our veterans what I say to new Cabinet members: Welcome aboard."
 A few weeks later, President Reagan delivered the following remarks at the Tomb of the Unknown Soldier in honor of Veterans Day, "Those who live today remember those who do not. Those who know freedom remember today those who gave up life for freedom. Today, in honor of the dead, we conduct ceremonies. We lay wreaths. We speak words of tribute. And in our memories, in our hearts, we hold them close to us still. Yet we also know, even as their families knew when they last looked upon them, that they can never be fully ours again, that they belong now to God and to that for which they so selflessly made a final and eternal act of devotion. We could not forget them. Even if they were not our own, we could not forget them. For all time, they are what we can only aspire to be: giving, unselfish, the epitome of human love -- to lay down one's life so that others might live. We think on their lives. We think on their final moments. In our mind's eye, we see young Americans in a European forest or on an Asian island or at sea or in aerial combat. And as life expired, we know that those who could had last thoughts of us and of their love for us. As they thought of us then, so, too, we think of them now, with love, with devotion, and with faith: the certainty that what they died for was worthy of their sacrifice -- faith, too, in God and in the Nation that has pledged itself to His work and to the dream of human freedom, and a nation, too, that today and always pledges itself to their eternal memory".
A few weeks later, President Reagan delivered the following remarks at the Tomb of the Unknown Soldier in honor of Veterans Day, "Those who live today remember those who do not. Those who know freedom remember today those who gave up life for freedom. Today, in honor of the dead, we conduct ceremonies. We lay wreaths. We speak words of tribute. And in our memories, in our hearts, we hold them close to us still. Yet we also know, even as their families knew when they last looked upon them, that they can never be fully ours again, that they belong now to God and to that for which they so selflessly made a final and eternal act of devotion. We could not forget them. Even if they were not our own, we could not forget them. For all time, they are what we can only aspire to be: giving, unselfish, the epitome of human love -- to lay down one's life so that others might live. We think on their lives. We think on their final moments. In our mind's eye, we see young Americans in a European forest or on an Asian island or at sea or in aerial combat. And as life expired, we know that those who could had last thoughts of us and of their love for us. As they thought of us then, so, too, we think of them now, with love, with devotion, and with faith: the certainty that what they died for was worthy of their sacrifice -- faith, too, in God and in the Nation that has pledged itself to His work and to the dream of human freedom, and a nation, too, that today and always pledges itself to their eternal memory".
The law delayed full implementation of the Act to March 1989, allowing the new incoming president to appoint a leader of his choice for the new department. Consequently, VA acknowledges both dates—when the law was signed/enacted and when it became fully effective—as significant markers in its history. On January 20, 1989, coinciding with his inauguration as the 41st president of the United States, George H. W. Bush appointed Edward J. Derwinski—a World War II veteran and twelve-term Congressman—as the last VA Administrator and the first Secretary of the newly formed Department of Veterans Affairs. President Bush praised the establishment of the new Department, stating, "There is only one place for the Veterans of America: in the Cabinet Room, at the table with the President of the United States of America." The transition took effect on March 15, 1989, leading to administrative changes at all levels. In keeping with tradition, the Department of Veterans Affairs continued using the abbreviation VA, a familiar term for veterans and others for nearly sixty years. Secretary Derwinski decided to maintain the “VA” name for the new department."

In August 1990 Iraq invaded Kuwait and seized control of that country. The United Nations Security Council condemned Iraq's invasion and called for the immediate and unconditional withdrawal of Iraqi forces. The invasion triggered a United States response to build a coalition of allies to deter an invasion of Saudi Arabia, free Kuwait from Iraqi occupation, and restore Kuwait's legitimate government. More than 500,000 American troops deployed to Saudi Arabia as part of Operation Desert Shield, in case Iraqi troops attacked Saudi Arabia. On 17 January 1991, Operation Desert Shield became Operation Desert Storm, backed by public support after diplomacy failed. About 697,000 U.S. troops took part in the war, with 299 losing their lives. The coalition forces, which included half a million American men and women, succeeded in all of its objectives.  During an Address Before a Joint Session of the Congress on the Cessation of the Persian Gulf Conflict on March 6, 1991, President Bush said, "All of us grieve for the victims of war, for the people of Kuwait and the suffering that scars the soul of that proud nation. We grieve for all our fallen soldiers and their families, for all the innocents caught up in this conflict. And, yes, we grieve for the people of Iraq, a people who have never been our enemy. My hope is that one day we will once again welcome them as friends into the community of nations. Our commitment to peace in the Middle East does not end with the liberation of Kuwait." Operation Desert Storm was the first major foreign crisis for the United States after the end of the Cold War. Desert Storm became the largest air campaign since the conflict in Southeast Asia. Veterans Health Services and Research Administration was changed to the Veterans Health Administration (VHA) in 1991. VA's National Center for PTSD, created in 1989 by an act of Congress, were an outstanding contribution to the war effort during Desert Shield/Storm.
During an Address Before a Joint Session of the Congress on the Cessation of the Persian Gulf Conflict on March 6, 1991, President Bush said, "All of us grieve for the victims of war, for the people of Kuwait and the suffering that scars the soul of that proud nation. We grieve for all our fallen soldiers and their families, for all the innocents caught up in this conflict. And, yes, we grieve for the people of Iraq, a people who have never been our enemy. My hope is that one day we will once again welcome them as friends into the community of nations. Our commitment to peace in the Middle East does not end with the liberation of Kuwait." Operation Desert Storm was the first major foreign crisis for the United States after the end of the Cold War. Desert Storm became the largest air campaign since the conflict in Southeast Asia. Veterans Health Services and Research Administration was changed to the Veterans Health Administration (VHA) in 1991. VA's National Center for PTSD, created in 1989 by an act of Congress, were an outstanding contribution to the war effort during Desert Shield/Storm.
VA Home Loan eligibility expanded for active Armed Forces members serving in the Persian Gulf War, including the National Guard and Reserve Forces after 90 days of active-duty wartime service. Persian Gulf War Veterans and eligible dependents became eligible for non-service-connected pension benefits in August of 1991. That same year, service-connected presumption of Persian Gulf War Veterans suffering psychosis within two years after discharge was extended health care benefits. In 1992, Congress authorized medical care for Persian Gulf War Veterans for conditions possibly related to exposure to toxic substances or environmental hazards. The Gulf War stands as a testament to the dedication and spirit of America’s military members and their willingness to fight for liberty and justice - anywhere and for anyone. Naval forces have transited the Persian Gulf region since 1801, and the reasons behind stationing a permanent naval presence since 1948 was revalidated by Desert Storm.
Anchorage Alaska VA Healthcare System was opened in 1992 and a partnership was established with VA and Indian Health Service. The "Indian Health Amendments of 1992." reauthorized appropriations for health services for American Indians and Alaska Natives. Alaska VA Healthcare System expanded health care access to rural areas, including 229 tribes. VA's Alaska Healthcare System provides Veterans with outstanding health care, trains America’s future health care providers, and conducts important medical research. VA Alaska Healthcare System provides Veterans with health care services at seven locations in Alaska including Anchorage VA Medical Center. VA Alaska Healthcare System maintain a 50-bed Domiciliary Residential Treatment Program and a 24-bed Compensative Work Therapy Transitional Residence Program. VA Alaska health care provides six CBOCs at Fort Wainwright in Fairbanks, at Joint Base Elmendorf-Richardson in Anchorage, and in Homer, Juneau, Soldotna, and Wasilla. In 1997, Alaska's first Director of Veterans Affairs was appointed. A Joint Venture was developed as a sharing agreement between the Anchorage VA clinic and the Joint Base Elmendorf-Richardson (JBER) base in 1999.
 Defense POW/MIA Accounting Agency was established in 1993 and serves as the central point in all policy matters on the POW/MIA issue within the DoD. Since 1973, the remains of over 1,000 Americans who died during the Vietnam War have been identified and returned to their families for burial with full military honors. Among the nearly 1,600 Americans still missing from the Vietnam War, hundreds are classified as “non-recoverable,” indicating that after extensive investigation, the Defense POW/MIA Accounting Agency has concluded that the individual perished but believes it is not possible to recover the remains. There were 766 prisoners of war, of whom 114 died in captivity. Occasionally, new leads can reactivate a case. National POW/MIA Recognition Day, observed on the third Friday in September, pays tribute to U.S. service members who were prisoners of war and those still missing in action from every conflict since World War II. Since the revival of U.S. POW/MIA recovery efforts in the 1970s, nearly 1,000 Americans who perished during World War II have been identified and returned to their families for interment with full military honors. This number complements the approximately 280,000 Americans whose remains were identified in a large-scale effort immediately after the war.
Defense POW/MIA Accounting Agency was established in 1993 and serves as the central point in all policy matters on the POW/MIA issue within the DoD. Since 1973, the remains of over 1,000 Americans who died during the Vietnam War have been identified and returned to their families for burial with full military honors. Among the nearly 1,600 Americans still missing from the Vietnam War, hundreds are classified as “non-recoverable,” indicating that after extensive investigation, the Defense POW/MIA Accounting Agency has concluded that the individual perished but believes it is not possible to recover the remains. There were 766 prisoners of war, of whom 114 died in captivity. Occasionally, new leads can reactivate a case. National POW/MIA Recognition Day, observed on the third Friday in September, pays tribute to U.S. service members who were prisoners of war and those still missing in action from every conflict since World War II. Since the revival of U.S. POW/MIA recovery efforts in the 1970s, nearly 1,000 Americans who perished during World War II have been identified and returned to their families for interment with full military honors. This number complements the approximately 280,000 Americans whose remains were identified in a large-scale effort immediately after the war.
At the time of Persian Gulf War Veterans' Benefits Act approval in 1994, it was not known whether these Servicemembers were exposed to chemical or biological warfare agents. However, threats of enemy use of chemical and biological warfare heightened the psychological stress associated with the military operation. During the Persian Gulf War, members of the U.S. Armed Forces were exposed to exposed to numerous potentially toxic substances, including fumes and smoke from military operations, oil well fires, diesel exhaust, paints, pesticides, depleted uranium, infectious agents, investigational drugs and vaccines, and indigenous diseases, and were also given multiple immunizations. Threats of enemy use of chemical and biological warfare heightened the psychological stress associated with the military operation. The purpose of the Persian Gulf War Veterans' Benefits Act was to promote greater outreach to Persian Gulf War veterans and their families to inform them of ongoing research activities, as well as the services and benefits to which they are currently entitled. This included compensation to Persian Gulf War veterans suffering disabilities resulting from illnesses.
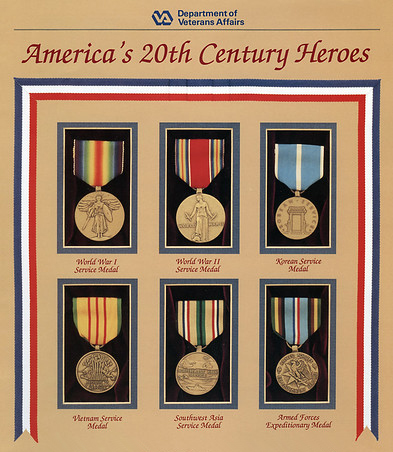 For VA benefit purposes, the term Persian Gulf Veteran means a Veteran who served on active military, naval, or air service in the Southwest Asia theater of operations during the Persian Gulf War. The Southwest Asia theater of operations refers to Iraq, Kuwait, Saudi Arabia, the neutral zone between Iraq and Saudi Arabia, Bahrain, Qatar, the United Arab Emirates, Oman, the Gulf of Aden, the Gulf of Oman, the Persian Gulf, the Arabian Sea, the Red Sea, and the airspace above these locations. The accelerated rate of deployments, family separations, and the stress of peacekeeping operations may have contributed to substantial psychopathology among active-duty, reservist, and Veteran personnel. Wartime compensation for Persian Gulf War Veterans was passed into law in 1994 for service-connected disability or death. As Operation Southern Watch continued, disaster struck the airmen serving in Southwest Asia.
For VA benefit purposes, the term Persian Gulf Veteran means a Veteran who served on active military, naval, or air service in the Southwest Asia theater of operations during the Persian Gulf War. The Southwest Asia theater of operations refers to Iraq, Kuwait, Saudi Arabia, the neutral zone between Iraq and Saudi Arabia, Bahrain, Qatar, the United Arab Emirates, Oman, the Gulf of Aden, the Gulf of Oman, the Persian Gulf, the Arabian Sea, the Red Sea, and the airspace above these locations. The accelerated rate of deployments, family separations, and the stress of peacekeeping operations may have contributed to substantial psychopathology among active-duty, reservist, and Veteran personnel. Wartime compensation for Persian Gulf War Veterans was passed into law in 1994 for service-connected disability or death. As Operation Southern Watch continued, disaster struck the airmen serving in Southwest Asia.
On June 25, 1996, terrorists bombed the Khobar Towers barracks on Dhahran Airbase in Saudi Arabia, killing 19 airmen and wounding 547 personnel. Undeterred by the terrorist attack, the U.S. Armed Forces continued to support Operation Southern Watch through the 1990s and early 2000s and coalition aircraft participated in Operations Desert Strike and Desert Fox, which targeted missile and weapons of mass destruction production sites in Iraq. VHA launched the first treatment trials for Gulf War Veterans in 1999 with focus on antibiotics and exercise. In August of 2000, terrorists detonated an inflatable speedboat alongside the USS Cole, killing 17 U.S. Navy Sailors. Drawing upon their Navy training and discipline, the crew of USS Cole heroically conducted more than 96 hours of sustained damage control in conditions of extreme heat and stress. Operation Southern Watch continued until March of 2003, when the United States began OIF. In the fall of 1996, VA expanded eligibility for readjustment counseling and certain related counseling services. The expansion included counseling of general mental and psychological assessment of combat Veterans. This expansion included any Veteran who served on active-duty in a theater of combat operations during the Vietnam War. Expansion also includued Veterans who served in the active military, naval, or air service in a theater of combat operations during a period of war, or in any other area during a period in which hostilities occurred in such area to assist the Veteran in readjusting to civilian life.
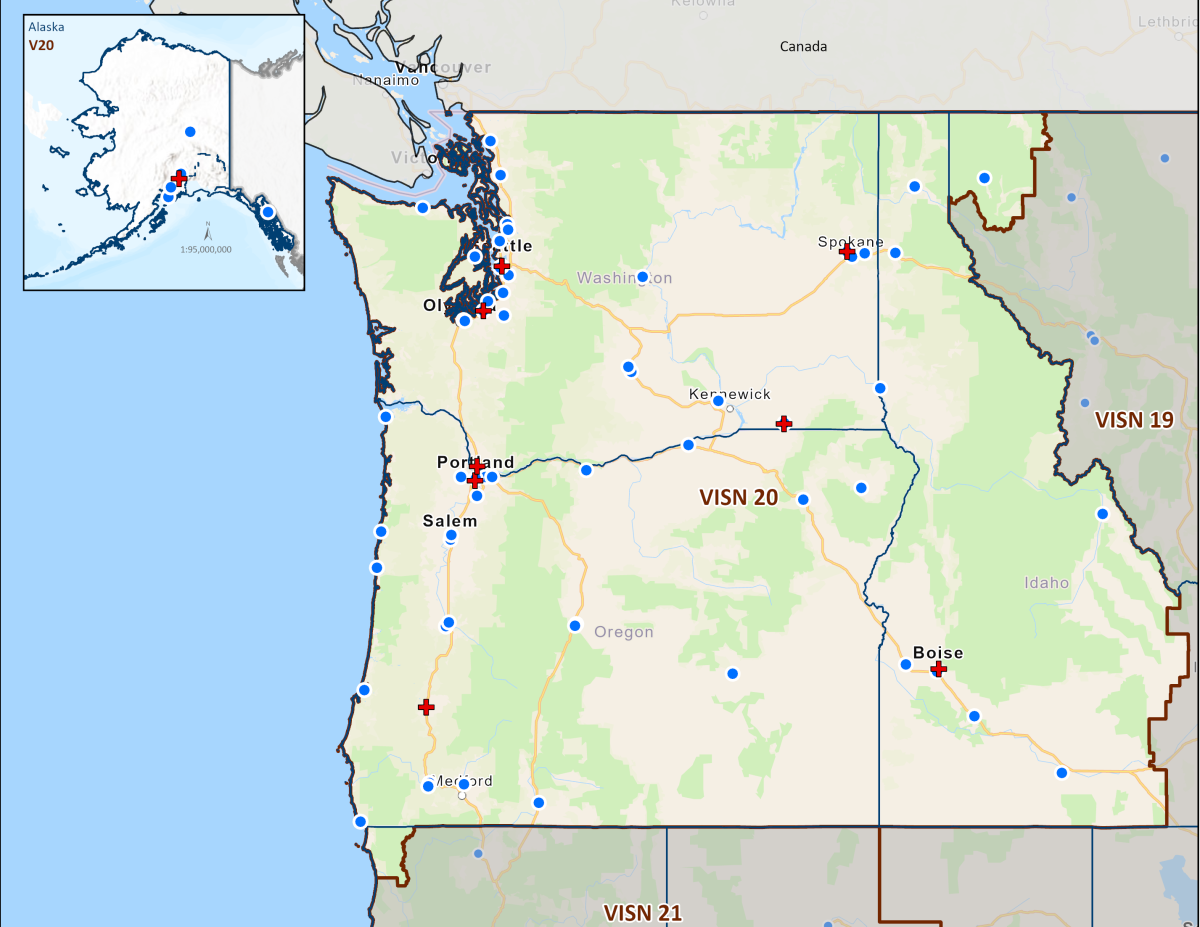 In 1997, the VA launched a series of specialized mental health centers designated to improve patient function and clinical understanding of mental illness. The centers, called "mental illness research, education and clinical centers," or MIRECCs, were modeled after the VA's geriatric research, education and clinical centers (GRECCs). Legislation had been introduced in Congress since 1988 to authorize the VA MIRECCs. The 104th Congress authorized the VA's MIRECCs in Public Law (Pub.L.) 104-262, Section 334, which was codified at 38 U.S.C. Sec. 7320. Mental health clinicians and VSOs had been advocates for MIRECCs for over a decade. VA Medical Centers in Puget Sound, Washington; Portland, Oregon; and Boise, Idaho VA Medical Centers were commissioned by Congress and VA to establish one of the first three Mental Illness Research, Education, and Clinical Centers (MIRECCs) in the United States.
In 1997, the VA launched a series of specialized mental health centers designated to improve patient function and clinical understanding of mental illness. The centers, called "mental illness research, education and clinical centers," or MIRECCs, were modeled after the VA's geriatric research, education and clinical centers (GRECCs). Legislation had been introduced in Congress since 1988 to authorize the VA MIRECCs. The 104th Congress authorized the VA's MIRECCs in Public Law (Pub.L.) 104-262, Section 334, which was codified at 38 U.S.C. Sec. 7320. Mental health clinicians and VSOs had been advocates for MIRECCs for over a decade. VA Medical Centers in Puget Sound, Washington; Portland, Oregon; and Boise, Idaho VA Medical Centers were commissioned by Congress and VA to establish one of the first three Mental Illness Research, Education, and Clinical Centers (MIRECCs) in the United States.
VA's VISN 20 MIRECC was founded on a conceptual framework embracing innovation and collaboration to improve quality in Veteran-centered behavioral disorder research, education and clinical care. NW MIRECC academic affiliates are UW and OHSU. MIRECC's were founded upon "an arrangement with an accredited medical school that provides education and training in psychiatry and with which one or more of the participating Department facilities is affiliated under which medical residents receive education and training in psychiatry through regular rotation through the participating Department facilities so as to provide such residents with training in the diagnosis and treatment of mental illness". The history of NW MIRECC began with VISN 20 clinicians and researchers working late on a cool March night to draft the NW MIRECC charter, envisioning a collaborative approach to research, education, and clinical care that would better support Veterans.
VA's NW MIRECC serves to improve the mental health and well-being of Veterans through research and dissemination of information to providers both within VA and the general public. The arrangement included accredited graduate program of psychology, along with nursing, social work, counseling, and allied health personnel for training and education in mental health. Additional MIRECCs initially stood up in 1997 were VISN 1 (Connecticut and Massachusetts) and VISN 22 (Southern California and Nevada). All sites were selected through a competitive peer-review process involving VA and other government and private-sector mental health professionals. VA MIRECC's provide for the improvement of the provision of health-care services and related counseling services to eligible Veterans suffering from mental illness (especially mental illness related to service-related conditions) through—

- the conduct of research (including research on improving mental health service facilities of the Department and on improving the delivery of mental health services by the Department);
- the education and training of health care personnel of the Department; and
- the development of improved models and systems for the furnishing of mental health services by the Department.
The initial goals of VISN 20 NW MIRECC were to discover and disseminate new knowledge about the neurobiology and clinical treatment of major mental disorders afflicting veterans. MIRECC scientists, educators and clinicians began by addressing four major areas:
- schizophrenia
- PTSD
- agitation and psychosis in Alzheimer's disease
- mental illness complicating chronic medical illness
The mission focus of the Northwest MIRECC is “the invisible wounds of war” posttraumatic stress disorder (PTSD) and blast-induced mild traumatic brain injury (mTBI) and their complex comorbidities including substance use disorders, chronic pain, and neurodegeneration and dementia. PTSD and mTBI comorbidities include alcohol use disorder (AUD), chronic pain (chronic postconcussive headache), cognitive impairment, and increased risk for neurodegenerative disorders (chronic traumatic encephalopathy [CTE] and Alzheimer's disease). NW MIRECC Research studies have significantly contributed to advancements in our understanding of medical problems and that have led to health improvements for Veterans and civilians alike. NW MIRECC applies a modern genetic, neurologic, and clinical trial methodology to the discovery and development of new and more effective treatments for major and often treatment-resistant mental disorders.
From its early days, NW MIRECC has conducted research to understand PTSD, TBI, schizophrenia, and other mental health challenges facing Veterans, including Alzheimer’s disease. That emphasis led to genetic discoveries in schizophrenia and the identification of cerebrospinal fluid (CSF) biomarkers for disruptive agitation in Alzheimer's disease. These findings were then passed on to clinicians and other VA personnel via MIRECC Presents, an accredited Continuing Education series on mental health topics provided by NW MIRECC. The VA ranks as one of the nation's leaders in health research. The VA's MIRECC system and its early achievements attracted positive attention at the National Institute of Mental Health (NIMH), National Institute on Drug Abuse (NIDA), Substance Abuse and Mental Health Services Administration (SAMHSA), Center for Mental Health Services (CMHS) and the Center for Substance Abuse Treatment (CSAT) with early offers of collaboration. VHA designated enhancement funds establishing the VA Centers of Excellence in Substance Addiction Treatment and Education (CESATE), including the Seattle CESATE located within the Seattle Division of VAPSHCS. In 1999, the VA's MIRECCs were featured at the American Psychiatric Association (APA) May meeting. MIRECCs were also featured at the major meetings of the APA and Society for Biological Psychiatry.
 Several compelling factors motivated VISN 20 MIRECC to focus on military PTSD and its complex comorbidities. First, the surge home of the "new" Veterans from OEF, OIF and OND added substantially to the already large number of Veterans of the Vietnam War and other conflicts struggling with the distress and functional impairments of PTSD and its comorbidities. Second, the close geographic proximity (40 miles) of DoD Joint Base Lewis McChord/Madigan Healthcare System (JBLM/MHS) to VA Puget Sound has provided the MIRECC the important opportunity to develop innovative and productive research, education and clinical care collaborations with the Department of Defense to address military PTSD and its comorbidities in their early stages in active duty Service Members. Third, during MIRECC clinicians’ provision of care to Veterans and Service Members, it became clear that PTSD is usually complicated by at least one and often multiple comorbid conditions. A typical OEF/OIF/OND combat Veteran with PTSD is also experiencing persistent postconcussive symptoms (such as chronic headache) from one or multiple mTBIs; is struggling with chronic musculoskeletal pain; is using alcohol excessively to relieve symptoms; and is increasingly concerned that their subjective cognitive symptoms will develop into dementia. These PTSD comorbidities also are common among Vietnam War and other era Veterans.
Several compelling factors motivated VISN 20 MIRECC to focus on military PTSD and its complex comorbidities. First, the surge home of the "new" Veterans from OEF, OIF and OND added substantially to the already large number of Veterans of the Vietnam War and other conflicts struggling with the distress and functional impairments of PTSD and its comorbidities. Second, the close geographic proximity (40 miles) of DoD Joint Base Lewis McChord/Madigan Healthcare System (JBLM/MHS) to VA Puget Sound has provided the MIRECC the important opportunity to develop innovative and productive research, education and clinical care collaborations with the Department of Defense to address military PTSD and its comorbidities in their early stages in active duty Service Members. Third, during MIRECC clinicians’ provision of care to Veterans and Service Members, it became clear that PTSD is usually complicated by at least one and often multiple comorbid conditions. A typical OEF/OIF/OND combat Veteran with PTSD is also experiencing persistent postconcussive symptoms (such as chronic headache) from one or multiple mTBIs; is struggling with chronic musculoskeletal pain; is using alcohol excessively to relieve symptoms; and is increasingly concerned that their subjective cognitive symptoms will develop into dementia. These PTSD comorbidities also are common among Vietnam War and other era Veterans.
As one of four statutory missions, the VA educates and trains health professionals to enhance the quality of and timely access to care provided to Veterans within VHA's healthcare system. To achieve this mission, "To educate for VA and the Nation", the VA has conducted health professions education and training in partnership with affiliated U.S. academic institutions in accordance with the landmark 1946 Policy Memorandum No. 2. Title 38 U.S.C. Section 7302 mandates that VA assist in carrying out a “program of education and training of health personnel; for its own needs and those of the nation. NW MIRECC produced a Best Practices Manual for PTSD. The CD-ROM independent study program was widely disseminated across the VA to complement the manual. VA Boise and VA Puget Sound MIRECC faculty collaborated with the Office of the Chairman Joint Chiefs of Staff to produce training and education films about PTSD and mTBI in OIF/OEF returnees as well as older veterans.
 As outlined in the charter of the Research Advisory Committee on Gulf War Veterans' Illnesses, the core principle guiding the Committee's work is that the main objective of Gulf War-related government research is to enhance the health of ill Gulf War Veterans. Established by Congress in 1998, the Committee was first appointed by Secretary of Veterans Affairs Anthony J. Principi in January 2002. VHA provides eligible Veterans with a Gulf War Registry health exam to detect any possible long-term health issues associated with Persian Gulf War service. Additionally, Persian Gulf War Veterans can apply to establish service connection for other "non-presumptive" diseases and illnesses linked to their service in the theater of operations. Some illnesses and conditions are designated by the VA as "presumed" to be related to military service in specified areas of Southwest Asia, potentially qualifying war Veterans for VA disability compensation benefits.
As outlined in the charter of the Research Advisory Committee on Gulf War Veterans' Illnesses, the core principle guiding the Committee's work is that the main objective of Gulf War-related government research is to enhance the health of ill Gulf War Veterans. Established by Congress in 1998, the Committee was first appointed by Secretary of Veterans Affairs Anthony J. Principi in January 2002. VHA provides eligible Veterans with a Gulf War Registry health exam to detect any possible long-term health issues associated with Persian Gulf War service. Additionally, Persian Gulf War Veterans can apply to establish service connection for other "non-presumptive" diseases and illnesses linked to their service in the theater of operations. Some illnesses and conditions are designated by the VA as "presumed" to be related to military service in specified areas of Southwest Asia, potentially qualifying war Veterans for VA disability compensation benefits.
The Gulf War Registry Health Exam informs Veterans of potential long-term health problems due to environmental exposures during military service. Medically unexplained illnesses (often known as Gulf War illness or Chronic Multi-symptom illness) are a major concern for some Veterans who served in the Persian Gulf War. It is important to note that the Persian Gulf War Registry health exam is distinct from VA disability benefits awarded for a presumptive disability or other service-connected conditions. The VA has extended the presumptive period to Dec. 31, 2026, for qualifying chronic disabilities rated 10% or more resulting from undiagnosed illnesses in Persian Gulf War Veterans.
![American flag over the side of the Pentagon as rescue and recovery efforts continued following the September 11, 2001 terrorist attack The original finding aid described this photograph as: [Complete] Scene Caption: Soldiers from the 3rd Infantry render honors as fire fighters and rescue workers unfurl a huge American flag over the side of the Pentagon as rescue and recovery efforts continued following the September 11, 2001 terrorist attack. The flag, a garrison flag, sent from the US Army Band at nearby Fort Myer, Virginia, is the largest authorized (20 x 38) flag for the military. Shortly after 8 AM on September 11, 2001 in an attempt to frighten the American people, five members of Al-Qaida, a group of fundamentalist Islamic Muslims, hijacked American Airlines Flight 77, a Boeing 757-200, from Dulles International Airport just outside Washington DC. About 9:30 AM they flew the aircraft and 64 passengers into the side of the Pentagon. The impact destroyed or damaged four of the five](https://www.mirecc.va.gov/visn20/images/9-11-pentagon-flag.jpeg) On September 11, 2001, terrorists flew commercial airliners into the World Trade Center's Twin Towers in New York City, the Pentagon in Arlington, Virginia, and downed Flight 93 in a field near Shanksville, Pennsylvania. There were 2,996 American lives lost, almost 600 more than Pearl Harbor on December 7, 1941. Forty-one Veterans and six family members of Veterans were laid to rest in national cemeteries. Those we lost on September 11, 2001, will forever hold a cherished place in our hearts and the history of our nation. Hundreds of thousands of people in the New York City (NYC) Disaster Area, at the Pentagon, and the crash site in Shanksville, PA were exposed to dust, debris, traumatic events, and physically and emotionally stressful conditions on and after September 11, 2001. Workers and volunteers performed rescue, recovery, clean-up, and other related support services in the disaster areas. By a joint resolution (Public Law 107-89), Congress authorized the President to designate September 11 of each year as "Patriot Day" to perpetuate the memory of those who perished in the attack on America, and to pursue peace and justice in the world and security at home. After the 9/11 attacks, DoD created a new civilian medal for personnel. The Defense of Freedom Medal is the civilian equivalent of the Purple Heart, awarded to DoD civilian employees who are killed or wounded by hostile action while serving in support of the department.
On September 11, 2001, terrorists flew commercial airliners into the World Trade Center's Twin Towers in New York City, the Pentagon in Arlington, Virginia, and downed Flight 93 in a field near Shanksville, Pennsylvania. There were 2,996 American lives lost, almost 600 more than Pearl Harbor on December 7, 1941. Forty-one Veterans and six family members of Veterans were laid to rest in national cemeteries. Those we lost on September 11, 2001, will forever hold a cherished place in our hearts and the history of our nation. Hundreds of thousands of people in the New York City (NYC) Disaster Area, at the Pentagon, and the crash site in Shanksville, PA were exposed to dust, debris, traumatic events, and physically and emotionally stressful conditions on and after September 11, 2001. Workers and volunteers performed rescue, recovery, clean-up, and other related support services in the disaster areas. By a joint resolution (Public Law 107-89), Congress authorized the President to designate September 11 of each year as "Patriot Day" to perpetuate the memory of those who perished in the attack on America, and to pursue peace and justice in the world and security at home. After the 9/11 attacks, DoD created a new civilian medal for personnel. The Defense of Freedom Medal is the civilian equivalent of the Purple Heart, awarded to DoD civilian employees who are killed or wounded by hostile action while serving in support of the department.
The VA is the world's leading research and educational center of excellence on PTSD and traumatic stress. VHA continually evolves and cultivates ongoing cutting-edge medical research and innovation to improve the lives of America’s patriots. VA provides major funding initiatives for research on neurotrauma, chronic pain, and other health problems prevalent in combat-wounded Veterans returning from Iraq and Afghanistan. As part of the NW MIRECC mission to enhance access to mental health expertise, NW MIRECC collaborates and consults with other MIRECCs and Centers of Excellence, as well as with other VA, DoD, Federal, State departments of Veterans Affairs, community agencies, and experts. MIRECC disseminates mission-relevant knowledge through publications and continuing health care education programs across VISN 20 and nationally. Due in part to NW MIRECC's web-based and face-to-face educational outreach efforts, prazosin is now prescribed to over 100,000 Veterans and active-duty Servicemembers, and we continue to investigate its usefulness for other Veteran-related illnesses, including, for example, the post-concussive headaches that Veterans report as one of the most disabling symptoms of mTBI. VHA medical centers throughout the country offer advanced services such as organ transplants and plastic surgery through VHA's National Transplant Program. Lumbar punctures, which are used to obtain CSF, and which have been safely performed in the NW MIRECC for more than two decades.
 Since 2003, the VA has collaborated with the DoD and military treatment facilities (MTFs) to transition the health care of injured or ill service members of the Global War on Terrorism (GWOT) to VA medical facilities. GWoT operational names include Enduring Freedom, Iraqi Freedom, New Dawn, Freedom's Sentinel, Enduring Sentinel, and Inherent Resolve. MTF is the broad term to include medical centers, hospitals and ambulatory care clinics, including dental clinics. From the onset of Enduring Freedom in Afghanistan and Iraqi Freedom, the Northwest MIRECC has directed major resources to the neuropsychiatric disorders highly prevalent among combat-exposed OEF/OIF returnees (posttraumatic stress disorder [PTSD] and blast concussive mild traumatic brain injury [mTBI]), and to collaborations in research, educational and treatment efforts between the MIRECC and Department of Defense components locally (Madigan AMC/Fort Lewis) and nationally (Walter Reed AMC and the Office of the Chairman Joint Chiefs of Staff). VHA launched My HealtheVet nationwide as an online Personal Health Record for Veterans, active-duty service members, their dependents, and caregivers. The resources and tools offer Veterans greater control and understanding over health care and wellness.
Since 2003, the VA has collaborated with the DoD and military treatment facilities (MTFs) to transition the health care of injured or ill service members of the Global War on Terrorism (GWOT) to VA medical facilities. GWoT operational names include Enduring Freedom, Iraqi Freedom, New Dawn, Freedom's Sentinel, Enduring Sentinel, and Inherent Resolve. MTF is the broad term to include medical centers, hospitals and ambulatory care clinics, including dental clinics. From the onset of Enduring Freedom in Afghanistan and Iraqi Freedom, the Northwest MIRECC has directed major resources to the neuropsychiatric disorders highly prevalent among combat-exposed OEF/OIF returnees (posttraumatic stress disorder [PTSD] and blast concussive mild traumatic brain injury [mTBI]), and to collaborations in research, educational and treatment efforts between the MIRECC and Department of Defense components locally (Madigan AMC/Fort Lewis) and nationally (Walter Reed AMC and the Office of the Chairman Joint Chiefs of Staff). VHA launched My HealtheVet nationwide as an online Personal Health Record for Veterans, active-duty service members, their dependents, and caregivers. The resources and tools offer Veterans greater control and understanding over health care and wellness.
Partnering with Veteran and non-veteran volunteers as clinical research subjects, NW MIRECC develops and evaluates effective treatments for PTSD and its associated conditions, including mTBI, SUD, chronic musculoskeletal pain, post-concussive headaches, and dementia. NW MIRECC studies are conducted through clinical research and through translational research wherein teams of clinicians and scientists work side-by-side to characterize and model key features of clinical problems and then translate the findings from scientific theory or animal models into practical applications for Veterans. Early translational research efforts of NW MIRECC focused on treatment for PTSD and its substance abuse comorbidities (alcohol and tobacco); the chronic behavioral consequences of mTBI and its objective diagnosis through biomarkers; the elderly veteran with agitated dementia; and schizophrenia and the adverse metabolic consequences of antipsychotic drug therapy.
 One example of this renewed emphasis on PTSD and its associated conditions has been NW MIRECCs work with the blood pressure medication prazosin. MIRECC investigators discovered that the inexpensive generic drug prazosin (that blocks excessive responses to the “adrenaline” neurotransmitter norepinephrine) is highly effective for reducing and often eliminating PTSD trauma nightmares, sleep disruption and daytime hyperarousal and reexperiencing symptoms in combat veterans and in civilians. These results led DoD funding for a placebo-controlled prazosin trial in active-duty soldiers from OIF/OEF with Madigan AMC and Walter Reed AMC and a VA Cooperative Study of prazosin for combat trauma PTSD in veterans. Additionally, staff at the NW MIRECC pioneered the use of this medication to treat trauma-related nightmares, one of the most common symptoms of PTSD.
One example of this renewed emphasis on PTSD and its associated conditions has been NW MIRECCs work with the blood pressure medication prazosin. MIRECC investigators discovered that the inexpensive generic drug prazosin (that blocks excessive responses to the “adrenaline” neurotransmitter norepinephrine) is highly effective for reducing and often eliminating PTSD trauma nightmares, sleep disruption and daytime hyperarousal and reexperiencing symptoms in combat veterans and in civilians. These results led DoD funding for a placebo-controlled prazosin trial in active-duty soldiers from OIF/OEF with Madigan AMC and Walter Reed AMC and a VA Cooperative Study of prazosin for combat trauma PTSD in veterans. Additionally, staff at the NW MIRECC pioneered the use of this medication to treat trauma-related nightmares, one of the most common symptoms of PTSD.
DoD and VA launched a Pilot program at three MTFs of the Integrated Disability Evaluation System (IDES) in 2007. IDES is a joint disability evaluation process. Based on the success of the IDES pilot program, the integrated process expanded to all remaining worldwide locations and is available to all Service members. Service members determined to be unfit for duty receive a single set of disability ratings to determine the appropriate level of DoD and VA disability benefits. Integration with VA provides medically separated or retired Veterans with timely access to their benefits. New programs provide treatment for TBI, PTSD, suicide prevention, women Veterans, and more. In operation since 2007, VA’s National Suicide Prevention Hotline is a free, confidential resource for Veterans, service members, National Guard and Reserve members, even if they’re not enrolled in VA benefits or health care. In 2020, 988 was authorized as the new three-digit phone number. By calling or texting 988, Veterans connect with mental health professionals. Veterans can press “1” after dialing 988 to connect directly to the Veterans Crisis Lifeline. Continuing care after the call, chat, or text, Veterans Crisis Line responders can refer Veterans to a local suicide prevention coordinator (SPC). Available in each VA medical center across the country, SPCs can connect Veterans to the counseling and services they need.
 The Defense Health Agency's Recovery Coordination Program launched the National Resource Directory (NRD) in 2008 as a resource website that connects wounded warriors, Service Members, Veterans, their families, and caregivers to programs and services that support them. That same year, each branch of military service stood up Wounded Warrior Commands under the DoD Warrior Care Program (WCP) to proactively support wounded, ill, and injured Service members in their recovery and reintegration or transition to civilian life.
The Defense Health Agency's Recovery Coordination Program launched the National Resource Directory (NRD) in 2008 as a resource website that connects wounded warriors, Service Members, Veterans, their families, and caregivers to programs and services that support them. That same year, each branch of military service stood up Wounded Warrior Commands under the DoD Warrior Care Program (WCP) to proactively support wounded, ill, and injured Service members in their recovery and reintegration or transition to civilian life.
- U.S. Army Recovery Care Program (ARCP)
- U.S. Navy Wounded Warrior - Safe Harbor (NWW)
- U.S. Marine Corps Wounded Warrior Regiment (WWR)
- U.S. Air Force Wounded Warrior Program (AFW2)
- U.S. Special Operations Command (USSOCOM) Warrior Care Program - Care Coalition (WCP-CC)
Navy Wounded Warrior is open to service members and Veterans in the U.S. Navy and Coast Guard with serious, non-combat, or combat-related injuries and physical or psychological illnesses. VA, DoD, Military Services, and collaborating organizations mark Warrior Care Month in November of each year. Warrior Care Month highlights the strength and resilience – physically, mentally, and spiritually – of our wounded, ill, and injured service members and their families and caregivers. The DoD Warrior Care Recovery Coordination Program and military services’ Wounded Warrior Programs provide comprehensive resources to assist recovering Service members and support spouses, families, and caregivers to meet their needs and achieve their goals. The wounded, ill, and injured population is broad, and includes not just the visibly wounded or injured. Many of the Service members going through recovery are suffering through a serious illness or dealing with post-traumatic stress or traumatic brain injury. Adaptive sports and reconditioning activities help wound warriors develop and enhance their skills in multiple domains of wellness, which can transfer to the job market and lead to success in other areas of life.
It is important for wounded warriors to know that they are not alone; there is a community that supports them in their challenges and recognizes their success. Building connections, sharing resources, and finding strength together helps wounded warriors understand that they aren’t alone. Wounded warrior support build connections within the community to lessen the sense of isolation often felt by those members. NW MIRECC and VAPORHCS played a significant role in co-leading Oregon's post-deployment effort. PVAMC added additional Neuro-Psychologist staff to clinically identify and manage Veterans suffering from TBI. Working with Oregon Department of Veterans Affairs (ODVA) and ONG; NW MIRECC, VAPORHCS, and PVAMC contributed to the development of the ODVA website for a comprehensive resource directory for available services and materials. ODVA, founded in 1945, led outreach efforts for Service members including development of Unseen Injuries - Medical Information for Combat Veterans led by ODVA. Post Deployment Summits were held with various federal and state agencies, along with Veterans organizations. The Post Deployment Summits helped all aspects of Veterans return to civilian life. Oregon's post-deployment efforts received national recognition in both VA and ONG. NW MIRECC has adapted its mission to more readily address the most critical needs of Veterans in this region: PTSD and its associated conditions; mTBI, SUD, AUD, chronic pain, post-concussive headaches, and dementia.
 VHA operates one of the largest healthcare systems in the world and provides training for a majority of America’s medical, nursing, and allied health professionals. Roughly 60 percent of all medical residents obtain a portion of their training at VA hospitals, and VA medical research programs benefit society at large. First launched in 2009, Mobile Vet Centers (MVCs) are large vehicles used to provide outreach to eligible individuals in communities that are distant from existing services. Throughout the country, there are 83 MVCs with space for confidential counseling. VISN 20 MVCs are currently deployed in Idaho, Oregon, and Washington. MVCs can access records through an encrypted connection. With this capability, MVCs are often called upon to support VA in its important mission of providing emergency services in response to national emergencies and disasters.
VHA operates one of the largest healthcare systems in the world and provides training for a majority of America’s medical, nursing, and allied health professionals. Roughly 60 percent of all medical residents obtain a portion of their training at VA hospitals, and VA medical research programs benefit society at large. First launched in 2009, Mobile Vet Centers (MVCs) are large vehicles used to provide outreach to eligible individuals in communities that are distant from existing services. Throughout the country, there are 83 MVCs with space for confidential counseling. VISN 20 MVCs are currently deployed in Idaho, Oregon, and Washington. MVCs can access records through an encrypted connection. With this capability, MVCs are often called upon to support VA in its important mission of providing emergency services in response to national emergencies and disasters.
VHA's Community Living Centers (CLC) (VA Nursing Homes) are for Veterans who do not need hospital or nursing home care but cannot live alone because of medical or serious mental illness. VISN 20 CLC's (VA Nursing Homes) are located in Boise ID, Roseburg OR, Seattle WA, Spokane WA, Tacoma WA, and Vancouver WA. Veterans receive nursing home level of care at VA CLCs, which includes help with activities of daily living and skilled nursing and medical care. There are 21 State Veterans Home in the six states served by VISN 20. The VA's Domiciliary evolved from a "Soldiers' Home" to become an active clinical rehabilitation and treatment program for male and female Veterans and domiciliary programs are now integrated with the Mental Health Residential Rehabilitation Treatment Program (MH RRTPs). In 2010, VHA's Domiciliary Care programs and MH RRTPs were merged into a single system of residential care to become a Mental Health RRTP. The primary goal of the MH RRTP is to provide treatment and rehabilitation services to Veterans who have mental health and substance use disorders that are often complex and co-occur with medical concerns and psychosocial needs, such as employment and housing. Veterans may stay for a short time or, in rare instances, for the rest of their lives. MH RRTP is the umbrella term for the array of programs and services that comprise mental health residential care. The term MH RRTP refers to those programs currently designated as Domiciliary RRTPs which may include Domiciliary Care for Homeless Veterans, Domiciliary Substance Use Disorder Programs, Domiciliary PTSD Programs, General Domiciliary Programs (General DOM), and Compensated Work Therapy (CWT) – Transitional Residence (TR). MH RRTPs CWT-TR is designed for Veterans participating in Compensated Work Therapy and who are in the process of transitioning to successful independent community living. VHA also provides RRTP for Veterans to overcome SUD problems from AUD to life-threatening addiction.
VHA's Advanced Psychology Postdoctoral Fellowship in Mental Illness Research and Treatment (MIRT) is a two-year postdoctoral training program at VAPORHCS. The primary goal of the NW MIRECC Advanced Psychology Postdoctoral Fellowship program is to train and equip physicians, psychologists, and other allied health professionals with the knowledge and expertise to lead clinical research efforts that make lasting contributions to the lives of Veterans experiencing mental health challenges. NW MIRECC Postdoctoral fellows have the opportunity to provide individual and group psychotherapy, supervise doctoral-level trainees, and actively participate in weekly team meetings and PTSD consultations as junior colleagues. In collaboration with their mentors, NW MIRECC Advanced Psychology Postdoctoral Fellows develop and implement research projects, publish, present findings, write grants, and utilize the latest technology for educational activities and clinical service delivery. Throughout the two-year program, NW MIRECC fellows are trained in clinical and health systems research, advanced clinical care service delivery, and program administration in an interdisciplinary setting. Psychology Postdoctoral Fellows devote 75% of their time to research and education activities and 25% to clinical training.
 Medical innovations, vocational training for the disabled, home ownership, educational opportunities, and the establishment of national shrines for burial and memorialization are all products of the nation’s efforts to care for its Veterans. Each of these measures directly impact American life. In 2010 VA collaborated with DoD and National Institutes of Health (NIH) and published "common data elements" with research focused on TBI and PTSD. The following year, DoD's Health Program, through agreement with the U.S. Army Medical Research and Materiel Command (USAMRMC), developed the Federal Interagency Traumatic Brain Injury Research (FITBIR) Informatics System. FITBIR promotes collaboration, accelerate research, and advance knowledge on the characterization, prevention, diagnosis, and treatment of TBI. In 2011, DoD expanded Purple Heart eligibility for Servicemembers who suffered certain mTBI or concussions.
Medical innovations, vocational training for the disabled, home ownership, educational opportunities, and the establishment of national shrines for burial and memorialization are all products of the nation’s efforts to care for its Veterans. Each of these measures directly impact American life. In 2010 VA collaborated with DoD and National Institutes of Health (NIH) and published "common data elements" with research focused on TBI and PTSD. The following year, DoD's Health Program, through agreement with the U.S. Army Medical Research and Materiel Command (USAMRMC), developed the Federal Interagency Traumatic Brain Injury Research (FITBIR) Informatics System. FITBIR promotes collaboration, accelerate research, and advance knowledge on the characterization, prevention, diagnosis, and treatment of TBI. In 2011, DoD expanded Purple Heart eligibility for Servicemembers who suffered certain mTBI or concussions.
VA purchased an 8-acre parcel for Snake River Canyon National Cemetery in 2016. Snake River Canyon National Cemetery is the first national cemetery in Idaho. The parcel purchase is part of VA's National Cemetery Administration Rural Initiative to provide access to VA burial benefits for Veterans who reside in rural areas and who have not previously had reasonable access to a national or state Veterans cemetery. The first phase of construction began in June of 2017 and was completed in March 2020. On Veterans Day in 2017, the Veterans online shopping benefit for the four military exchanges, Army Air Force Exchange (AAFES), Navy Exchange Services Command (NEXCOM), Marine Corps Exchange (MCX), and Coast Guard Exchange (CGX), became effective. This lifelong benefit allows honorably discharged Veterans of all United States Armed Forces to shop online at any and all of the exchanges. Allowing online shopping is a way to recognize those who served honorably and allows Veterans to make a tangible contribution to the quality of life of those who remain on active-duty. VetVerify is a shared verification service of the four military exchanges (AAFES, NEXCOM, MCX and CGX) that supports the Veterans online shopping benefit by verifying Veterans who cannot be authenticated by the exchanges alone. VetVerify uses data from the Defense Manpower Data Center (DMDC) as well as other government sources of Veteran records to verify eligibility.
 In accordance with the 2017 National Defense Authorization Act, Puget Sound Military Health System (MHS) transitioned administration and management of all military hospitals and clinics from the military departments to the Defense Health Agency (DHA). The MHS collaboration with staff at Army, Navy and Air Force MTFs in the Pacific Northwest works with TRICARE partners, VA hospitals, other federal health care organizations, private sector teaching hospitals and medical universities, and other health care partners. In the Pacific Northwest the MHS includes U.S. Army Madigan Medical Center, Naval Hospital Bremerton, Naval Health Clinic Oak Harbor, Naval Station Everett clinic, and the 62nd Medical Squadron of the U.S. Air Force. TRICARE serves Uniformed Service members and their families, Army National Guard, Army Reserve, Navy Reserve, Marine Corps Reserve, Air National Guard, Air Force Reserve, U.S. Coast Guard Reserve and their families, Survivors, Former spouses, Medal of Honor recipients and their families, and others registered in the Defense Enrollment Eligibility Reporting System (DEERS).
In accordance with the 2017 National Defense Authorization Act, Puget Sound Military Health System (MHS) transitioned administration and management of all military hospitals and clinics from the military departments to the Defense Health Agency (DHA). The MHS collaboration with staff at Army, Navy and Air Force MTFs in the Pacific Northwest works with TRICARE partners, VA hospitals, other federal health care organizations, private sector teaching hospitals and medical universities, and other health care partners. In the Pacific Northwest the MHS includes U.S. Army Madigan Medical Center, Naval Hospital Bremerton, Naval Health Clinic Oak Harbor, Naval Station Everett clinic, and the 62nd Medical Squadron of the U.S. Air Force. TRICARE serves Uniformed Service members and their families, Army National Guard, Army Reserve, Navy Reserve, Marine Corps Reserve, Air National Guard, Air Force Reserve, U.S. Coast Guard Reserve and their families, Survivors, Former spouses, Medal of Honor recipients and their families, and others registered in the Defense Enrollment Eligibility Reporting System (DEERS).
The Defense Commissary Agency expanded the Commissary Benefit and shopping privileges as part of the Purple Heart and Disabled Veterans Equal Access Act, as part of the John S. McCain National Defense Authorization Act for Fiscal Year 2019. Starting on January 1, 2020, all service-connected disabled veterans, Purple Heart recipients, former prisoners of war and primary veteran caregivers became eligible to shop at commissaries worldwide. DoD, VA, and Department of Homeland Security (the expansion also applies to Coast Guard facilities) partnered to make the expansion possible. Details of eligibility and military installation access follow:

- Disabled and other eligible veterans: The Veteran Health Identification card (VHIC), with “Purple Heart,” “Former POW” or “Service Connected” printed on the front, will be required for access into the installation and entry to the stores.
- Caregivers: The benefit applies to the approved and designated primary family caregiver of service-connected disabled veterans who are registered in the Department of Veterans Affairs Program of Comprehensive Assistance for Family Caregivers to receive shopping privileges.
VA's Maintaining Internal Systems and Strengthening Integrated Outside Networks Act (MISSION Act) (Public Law 115-182), was enacted in 2018, created Veterans Community Care to replace the Veterans Choice Program. Eligible veterans may choose community care even if a VHA provider is available as long as they meet specific requirements. Types of care under VA Veterans Community Care include General Community Care, Urgent Care, Emergency Care, Foreign Medical Care, Home Health and Hospice Care, Indian and Tribal Health Services, In Vitro Fertilization, State Veterans Home, and Flu Shots. To be eligible for Veterans Community Care, you must meet requirements:
- You’re enrolled in or eligible for VA health care, and
- You have approval from your VA health care team before you get care from a community provider (except for certain cases like urgent or emergency care)
During a medical emergency, Veterans should immediately seek care at the nearest medical facility. Generally, emergency treatment is only covered until such time as the Veteran can be safely transferred to a VA or other federal facility. If the Veteran refuses to be transferred to a VA or other federal facility after their emergency condition is stabilized, they may be liable for the cost of care beyond the point of stabilization.
 In 2018 VA launched a telehealth program to serve Veterans living in rural areas who have PTSD. Veterans may be eligible for care through a provider in their local community depending on their healthcare needs or circumstances, and if they meet specific eligibility criteria. The U.S. Space Force was established in December 2019 creating the first new branch of the armed services in 73 years. The Air Force Wounded Warrior Program (Air Force and Space Force) works together. The establishment of the USSF resulted from widespread recognition that Space was a national security imperative. Guardians of the USSF protect and defend American interests and ensure our forces, our allies, and the world never experience a day without space. Also in 2019, VAPSHCS opened a new 220,000-square-foot Mental Health and Research Building on the Seattle Washington campus. The Seattle expansion provides outpatient mental health care services, from medication management and psychosocial case management to Dialectical Behavior Therapy and evidence-based individual, family, and group psychotherapy for all major mental health diagnoses. MIRECC clinical programs stress a "precision medicine" approach to treating combat Veterans suffering from PTSD, mTBI, and their common comorbidities. Precision medicine is an approach which aims to tailor disease prevention and treatment by taking into account differences in an individual’s clinical, lifestyle, genetic and biomarker information. In October 2021, the Office of Research and Development (ORD) and the Office of Mental Health and Suicide Prevention (OMHSP) convened an Expert Working Group comprised of renowned experts in the fields of mental health, structural, functional, molecular, and physiological brain and mental health biomarkers from VA MIRECCs and VA Clinical Science Research and Development/Rehabilitation Research and Development (CSR&D/RR&D) research community.
In 2018 VA launched a telehealth program to serve Veterans living in rural areas who have PTSD. Veterans may be eligible for care through a provider in their local community depending on their healthcare needs or circumstances, and if they meet specific eligibility criteria. The U.S. Space Force was established in December 2019 creating the first new branch of the armed services in 73 years. The Air Force Wounded Warrior Program (Air Force and Space Force) works together. The establishment of the USSF resulted from widespread recognition that Space was a national security imperative. Guardians of the USSF protect and defend American interests and ensure our forces, our allies, and the world never experience a day without space. Also in 2019, VAPSHCS opened a new 220,000-square-foot Mental Health and Research Building on the Seattle Washington campus. The Seattle expansion provides outpatient mental health care services, from medication management and psychosocial case management to Dialectical Behavior Therapy and evidence-based individual, family, and group psychotherapy for all major mental health diagnoses. MIRECC clinical programs stress a "precision medicine" approach to treating combat Veterans suffering from PTSD, mTBI, and their common comorbidities. Precision medicine is an approach which aims to tailor disease prevention and treatment by taking into account differences in an individual’s clinical, lifestyle, genetic and biomarker information. In October 2021, the Office of Research and Development (ORD) and the Office of Mental Health and Suicide Prevention (OMHSP) convened an Expert Working Group comprised of renowned experts in the fields of mental health, structural, functional, molecular, and physiological brain and mental health biomarkers from VA MIRECCs and VA Clinical Science Research and Development/Rehabilitation Research and Development (CSR&D/RR&D) research community.
VA's mission is to serve America’s Veterans and their families with dignity and compassion and be their principal advocate in ensuring that they receive medical care, benefits, social support, and lasting memorials. Today's VHA — the largest of the three administrations that comprise the VA — continues to meet Veterans' changing medical, surgical, and quality-of-life needs. VHA Medical Centers provide a wide range of services including traditional hospital-based services such as pharmacy, critical care, radiology, orthopedics, physical therapy, surgery, and mental health. VHA is the largest integrated health care system in the United States, providing care at 1,321 health care facilities, including 172 VA Medical Centers and 1,138 outpatient sites of care of varying complexity to over 9 million Veterans enrolled in VHA's health care programs. In 2023, VA announced the deployment of 25 Mobile Medical Units (MMUs) comprised of Ford F-550 Super Duty Trucks and Mercedes-Benz Sprinter Vans. As a result, VISN 20 deployed two MMUs in Washington. MMUs will provide health care and support to homeless and at-risk Veterans to meet with medical providers, including mental health clinicians, social workers, and staff. VHA's VISN 20 Mobile services include primary care, laboratory services, social work, nutrition, clinical pharmacist consultations, mental health, telehealth specialty services, prosthetics, and orthotics. In addition, most VA medical centers offer additional medical and surgical specialty services including audiology and speech pathology, dermatology, dental, geriatrics, neurology, oncology, podiatry, prosthetics, urology, and vision care.

VA promotes the honor, health, and dignity of all Veterans in recognition of their service to our nation. From 1775 through the 1991-1992 Gulf War, 41,892,128 Veterans have served in the U.S. Military during Wartime. Of those that served, 651,031 died in battle. Another 308,800 died in theater, and an additional 230,254 died in service (non-theater). As of November 2023, there are 19,210,000 Living Veterans (Periods of War & Peace). VA provides benefits to 5,641,175 service-connected Veterans and 155,148 non-service connected Veterans (Periods of War & Peace). For service-connected disability compensation and pension purposes, the Persian Gulf War period has not yet been terminated. Persian Gulf War operational names included Desert Shield, Desert Storm, Desert Sabre, Southern Watch, Provide Comfort, and Northern Watch. In addition, various phases of each operation may have a unique operational name. The Persian Gulf War period includes Veterans of Operation Enduring Freedom, Operation Iraqi Freedom, and Operation New Dawn.
VA continues to innovate and modernize to serve millions of America’s patriots and their families and beneficiaries. Often when service members leave the military, they find difficulty with a sense of identity, financial strain, employment/education barriers, relationship changes, mental/emotional wellness, and physical limitations as a result of their time in the military. Post-9/11 Transition and Case Management (TCM) ensures that transitioning service members and Veterans receive the care and support they need as they transition from military to civilian life. The Wounded, Ill, and/or Injured Compensation and Benefits Handbook for Service Members of the Armed Forces is a living document, updated annually by DOD in collaboration with VA, Labor, and Education, as well as the Social Security Administration and the U.S. military services. In recent years VHA has opened more CBOCs, established telemedicine, Vet Centers, and suicide prevention hotlines, and developed other services to accommodate a diverse and ever-changing Veteran population.
 Today’s VHA has roots spanning over 150 years and continues to meet Veterans’ changing medical, surgical, and quality of life needs. The services provided to Veterans affected American society and culture as much as the service rendered by Veterans. The Plymouth colony first cared for Veterans beginning in 1636. Three hundred and eighty-nine years later, the United States continues to provide the best possible care for our greatest assets. NW MIRECC reaffirms its commitment that there is no higher priority than caring for the wounded, ill, and injured service members who have sacrificed so much. NW MIRECC continues to be at the tip of the sword in response to Warrior Care and continues to strive to improve the health and well-being of our Veterans. There is no greater calling than to care for those who ensured our freedom; Warrior Care is America's duty.
Today’s VHA has roots spanning over 150 years and continues to meet Veterans’ changing medical, surgical, and quality of life needs. The services provided to Veterans affected American society and culture as much as the service rendered by Veterans. The Plymouth colony first cared for Veterans beginning in 1636. Three hundred and eighty-nine years later, the United States continues to provide the best possible care for our greatest assets. NW MIRECC reaffirms its commitment that there is no higher priority than caring for the wounded, ill, and injured service members who have sacrificed so much. NW MIRECC continues to be at the tip of the sword in response to Warrior Care and continues to strive to improve the health and well-being of our Veterans. There is no greater calling than to care for those who ensured our freedom; Warrior Care is America's duty.
NW MIRECC disseminates mission-relevant knowledge through publications and continuing health care education programs across VISN 20 and nationally. Sign up for email updates or access your subscriber preferences: https://public.govdelivery.com/accounts/USVHAVISN20/subscriber/new.
Use of these Materials and Finding VA Health Care
Please note that the health care information provided in these materials is for educational purposes only. It does not replace the role of a medical practitioner for advice on care and treatment. If you are looking for professional medical care, find your local VA healthcare center by using the VA Facilities Locator & Directory. This page may contain links that will take you outside of the Department of Veterans Affairs website. VA does not endorse and is not responsible for the content of the linked websites.
VA Web Disclaimers
Disclaimer of Endorsement: Reference herein to any specific commercial products, process, or service by trade name, trademark, manufacturer, or otherwise, does not necessarily constitute or imply its endorsement, recommendation, or favoring by the United States Government. The views and opinions of authors expressed herein do not necessarily state or reflect those of the United States Government, and shall not be used for advertising or product endorsement purposes.
Disclaimer of Hyperlinks: The appearance of external hyperlinks does not constitute endorsement by the Department of Veterans Affairs of the linked websites, or the information, products or services contained therein. For other than authorized VA activities, the Department does not exercise any editorial control over the information you may find at these locations. All links are provided with the intent of meeting the mission of the Department and the VA website. Please let us know about existing external links which you believe are inappropriate and about specific additional external links which you believe ought to be included.
Disclaimer of Liability: With respect to documents available from this server, neither the United States Government nor any of its employees, makes any warranty, express or implied, including the warranties of merchantability and fitness for a particular purpose, or assumes any legal liability or responsibility for the accuracy, completeness, or usefulness of any information, apparatus, product, or process disclosed, or represents that its use would not infringe privately owned rights.
Reference from this web page or from any of the information services sponsored by the VA to any non-governmental entity, product, service or information does not constitute an endorsement or recommendation by the VA or any of its employees. We are not responsible for the content of any "off-site" web pages referenced from this server.
Disclaimer: The sharing of any non-VA information does not constitute an endorsement of products or services on the part of the VA.
![]()
VA Regional Offices
 The Veterans Benefits Administration (VBA) helps service members transition out of military service, and assists with Veterans with education, home loans, life insurance and much more. Service members, Veterans, their families, and Survivors are invited to request information on VA Benefits including disability compensation, pension, fiduciary, education, Veteran Readiness and Employment (VR&E), Home Loans, and Insurance. In addition to information on VA Benefits Veterans may initiate an intent to file and request assistance with filing compensation and pension claims. Visit regional office websites to learn about the services the regional office provides, directions to the facility, hours of operation, and the leadership team that serves the regional office.
The Veterans Benefits Administration (VBA) helps service members transition out of military service, and assists with Veterans with education, home loans, life insurance and much more. Service members, Veterans, their families, and Survivors are invited to request information on VA Benefits including disability compensation, pension, fiduciary, education, Veteran Readiness and Employment (VR&E), Home Loans, and Insurance. In addition to information on VA Benefits Veterans may initiate an intent to file and request assistance with filing compensation and pension claims. Visit regional office websites to learn about the services the regional office provides, directions to the facility, hours of operation, and the leadership team that serves the regional office.
Find out if you can get VA health care as a Veteran
The following four categories of Veterans are not required to enroll but are urged to do so to permit better planning of health resources:
- Veterans with a service-connected (SC) disability rated at 50% or more.
- Veterans seeking care for a disability the military determined was incurred or aggravated in the line of duty, but which VA has not yet rated, within 12 months of discharge.
- Veterans seeking care for a SC disability only or under a special treatment authority.
- Veterans seeking health registry examinations. VA’s health registry evaluation is a free, voluntary medical assessment for Veterans who may have been exposed to certain environmental hazards during military service. The evaluations alert Veterans to possible long-term health problems that may be related to exposure to specific environmental hazards during their military service. VA has established several health registries to track and monitor the health of specific groups of Veterans. You may be eligible to participate in one or more of these health registries: Agent Orange Registry, Airborne Hazards and Open Burn Pit Registry, Gulf War Registry (includes Operations Iraqi Freedom and New Dawn), Ionizing Radiation Registry, Depleted Uranium Follow-Up Program, and Toxic Embedded Fragment Surveillance Center. Use the chart below to help determine your eligibility.
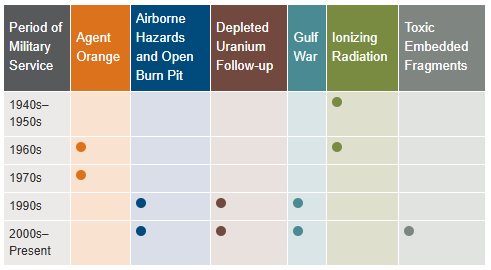
Find out how to apply for VA health care benefits as a Veteran or service member. For other mental health services, contact a VA medical center for information on eligibility and treatment options.
Community Care (Mission Act)
The MISSION Act became law in 2018, bringing the VA’s previous Veterans Choice Program to an end and establishing the Community Care Program. VA provides health care for Veterans from providers in your local community outside of VA. Veterans may be eligible to receive care from a community provider when VA cannot provide the care needed. This care is provided on behalf of and paid for by VA. Community care is also available to Veterans based on certain conditions and eligibility requirements, and in consideration of a Veteran’s specific needs and circumstances. VA offers urgent care services to eligible Veterans at in-network urgent care clinics to treat minor injuries and illnesses that are not life-threatening, such as colds, strep throat, sprained muscles, and skin and ear infections. Community care must be first authorized by VA before a Veteran can receive care from a community provider.
Vet Centers in VISN 20
 Vet Centers in VISN 20 are community-based counseling centers that provide a wide range of social and psychological services, including professional readjustment counseling to eligible Veterans, active-duty Army, Navy, Marine Corp, Air Force, Space Force, and Coast Guard service members, including National Guard and Reserve components, and their families. 1-877-927-8387 is an around the clock confidential call center where combat Veterans and their families can call to talk about their military experience or any other issue they are facing in their readjustment to civilian life. The staff is comprised of combat Veterans from several eras as well as families members of combat Veterans. This benefit is prepaid through the Veteran’s military service.
Vet Centers in VISN 20 are community-based counseling centers that provide a wide range of social and psychological services, including professional readjustment counseling to eligible Veterans, active-duty Army, Navy, Marine Corp, Air Force, Space Force, and Coast Guard service members, including National Guard and Reserve components, and their families. 1-877-927-8387 is an around the clock confidential call center where combat Veterans and their families can call to talk about their military experience or any other issue they are facing in their readjustment to civilian life. The staff is comprised of combat Veterans from several eras as well as families members of combat Veterans. This benefit is prepaid through the Veteran’s military service.
Alaska
| Anchorage Vet Center (Anchorage, AK) | Fairbanks Vet Center (Fairbanks, AK) |
| Kenai Vet Center Outstation (Soldotna, AK) | Wasilla Vet Center (Wasilla, AK) |
Idaho
| Boise Vet Center (Boise, ID) | East Idaho Vet Center (Idaho Falls, ID) |
Oregon
| Central Oregon Vet Center (Bend, OR) | Eugene Vet Center (Eugene, OR) |
| Grants Pass Vet Center (Grants Pass, OR) | Portland, OR Vet Center (Portland, OR) |
| Salem Vet Center (Salem, OR) |
Washington
Plan your trip to VA
 In 1946, Veterans Canteen Service (VCS) was established by law to provide comfort and well-being to America’s Veterans. With our many retail stores, cafés and coffee shops across the country, we serve those who have served our country. We are a self-sustaining entity providing merchandise and services to Veterans enrolled in VA’s healthcare system, their families, caregivers, VA employees, volunteers and visitors. We are honored to give back to the VA community through many programs established for the health and well-being of our nation’s heroes. Revenues generated from VCS are used to support a variety of programs, such as VA’s Rehabilitation Games, Fisher Houses, Poly-Trauma Centers for OIF/OEF/OND Veterans, disaster relief efforts, Substance Abuse Cessation, VA’s Homelessness initiatives, Women Veterans, Veteran Suicide Prevention and other activities.
In 1946, Veterans Canteen Service (VCS) was established by law to provide comfort and well-being to America’s Veterans. With our many retail stores, cafés and coffee shops across the country, we serve those who have served our country. We are a self-sustaining entity providing merchandise and services to Veterans enrolled in VA’s healthcare system, their families, caregivers, VA employees, volunteers and visitors. We are honored to give back to the VA community through many programs established for the health and well-being of our nation’s heroes. Revenues generated from VCS are used to support a variety of programs, such as VA’s Rehabilitation Games, Fisher Houses, Poly-Trauma Centers for OIF/OEF/OND Veterans, disaster relief efforts, Substance Abuse Cessation, VA’s Homelessness initiatives, Women Veterans, Veteran Suicide Prevention and other activities.
VCS operates over 200 Patriot Stores in Veterans Administration (VA) Medical Centers nationwide. Many of our stores have been recently updated and expanded to provide our customers with a modern, clean and comfortable shopping experience. Our stores welcome our customers with wider aisles, wood-like floors, enhanced lighting and directional signage. PatriotStores have expanded hours of operation to provide service for customers on weekends at most locations.
The Patriot Cafe is the best place in the VA Medical Center to enjoy delicious, freshly prepared breakfast or lunch served hot or cold each weekday. Providing Veterans, their families, VA employees, volunteers and visitors a place to relax and enjoy a meal or take-out for their convenience. With a wide variety of food from traditional comfort food, specialized menu selections and a large assortment of healthy choices; there is something for everyone's taste buds.
Hospital Service Directory
To find out whether there is a van near you use the Disabled American Veterans (DAV) Hospital Service Coordinator Directory to contact your nearest HSC for information or assistance. Please remember that the DAV Transportation Network is staffed by volunteers; therefore, it is unable to cover every community. The vans are driven by volunteers, and the rides coordinated by more than 133 Hospital Service Coordinators around the country. Our nation’s heroes travel around the globe to protect our freedoms—it’s only right that we return their dedication. Volunteering to drive a Vet ensures that even those living remotely from VA hospitals can make their appointments and never go without the treatment they need. Learn more about the DAV transportation network through the VISN 20 NewsFlash Resources section.
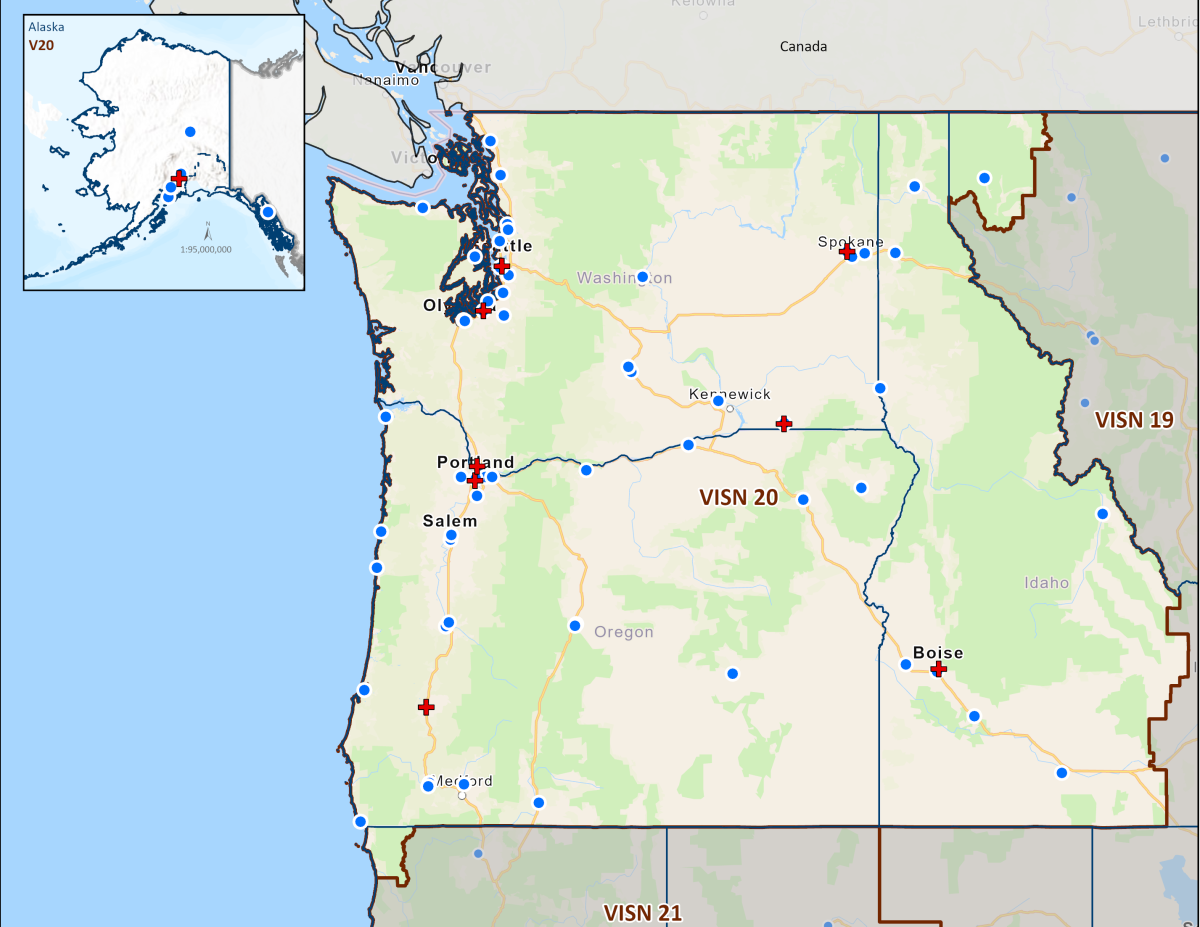 Today's VHA - the largest of the three administrations that comprise the VA - continues to meet Veterans' changing medical, surgical, and quality-of-life needs. VHA is the largest integrated health care system in the United States, providing care at 1,321 health care facilities, including 172 VA Medical Centers and 1,138 outpatient sites of care of varying complexity (VHA outpatient clinics) to over 9 million Veterans enrolled in the VA health care program. There are 18 Veterans Integrated Service Networks (VISNs) in VHA operating as regional systems of care to better meet local health care needs and provides greater access to care. In the Pacific Northwest, VISN 20 serves Veterans in Alaska, Oregon, Washington, most of Idaho, and one county each in California and Montana. Spanning 23% of the US land mass, VISN 20 is the largest geographic region of VA. Operating across three time zones over 817,417 square miles, VISN 20 is home to 273 federally recognized American Indian and Alaskan Native tribes. According to DoD, American Indians and Alaska Natives have one of the highest representations in the United States Armed Forces. VA consults with American Indian and Alaska Native tribal governments to develop partnerships that enhance access to services and benefits by Veterans and their families. VA is committed to ensuring that Native American Veterans and their families are able to utilize all benefits and services they are entitled to receive. As of the end of FY2024, 39% of VISN 20 enrollees resided in rural or highly rural areas.
Today's VHA - the largest of the three administrations that comprise the VA - continues to meet Veterans' changing medical, surgical, and quality-of-life needs. VHA is the largest integrated health care system in the United States, providing care at 1,321 health care facilities, including 172 VA Medical Centers and 1,138 outpatient sites of care of varying complexity (VHA outpatient clinics) to over 9 million Veterans enrolled in the VA health care program. There are 18 Veterans Integrated Service Networks (VISNs) in VHA operating as regional systems of care to better meet local health care needs and provides greater access to care. In the Pacific Northwest, VISN 20 serves Veterans in Alaska, Oregon, Washington, most of Idaho, and one county each in California and Montana. Spanning 23% of the US land mass, VISN 20 is the largest geographic region of VA. Operating across three time zones over 817,417 square miles, VISN 20 is home to 273 federally recognized American Indian and Alaskan Native tribes. According to DoD, American Indians and Alaska Natives have one of the highest representations in the United States Armed Forces. VA consults with American Indian and Alaska Native tribal governments to develop partnerships that enhance access to services and benefits by Veterans and their families. VA is committed to ensuring that Native American Veterans and their families are able to utilize all benefits and services they are entitled to receive. As of the end of FY2024, 39% of VISN 20 enrollees resided in rural or highly rural areas.
VA Medical Centers within VISN 20
Colonel Mary Louise Rasmuson Campus of the Alaska VA Healthcare System, Anchorage, Alaska
VA Boise Medical Center of the Boise VA Healthcare System, Boise, Idaho
VA Portland Medical Center of the Portland VA Healthcare System, Portland, Oregon
VA Roseburg Medical Center of the Roseburg VA Healthcare System, Roseburg, Oregon
VA White City Medical Center of the VA Southern Oregon Healthcare System, White City, Oregon
VA Seattle Medical Center of the VA Puget Sound Healthcare System, Seattle, Washington
Mann-Grandstaff Department of Veterans Affairs Medical Center, Spokane, Washington
Jonathan M. Wainwright Memorial VA Medical Center of the VA Walla Walla Healthcare System, Walla Walla, Washington
VA Puget Sound Health Care System (VAPSHCS) serves Veterans from a five-state area in the Pacific Northwest with two main divisions: American Lake VA Medical Center and Seattle VA Medical Center. Veterans Medical Centers are also located in Spokane, Vancouver, and Walla Walla. VA Outpatient Clinics and Vet Centers are located in Bellingham, Bellevue, Bremerton, Edmunds, Everett, Federal Way, Lacey, Mount Vernon, Olympia, Port Angeles, Puyallup, Richland, Renton, Silverdale, Seattle, Spokane, Union Gap, Vancouver, Walla Walla, Wenatchee, and Yakima.
VA Portland Health Care System (VAPORHCS) serves Veterans in Oregon and Southwest Washington with two main divisions: Portland VA Medical Center and Vancouver VA Medical Center. Veterans Medical Centers are also located in Roseburg, White City, and Vancouver, Washington. VA Outpatient Clinics and Vet Centers are located in Astoria, Bend, Boardman, Brookings, Eugene, Fairview, Grants Pass, Hines, Hillsboro, Klamath Falls, LaGrande, Lincoln City, Newport, Portland, Salem, The Dalles, and West Linn.
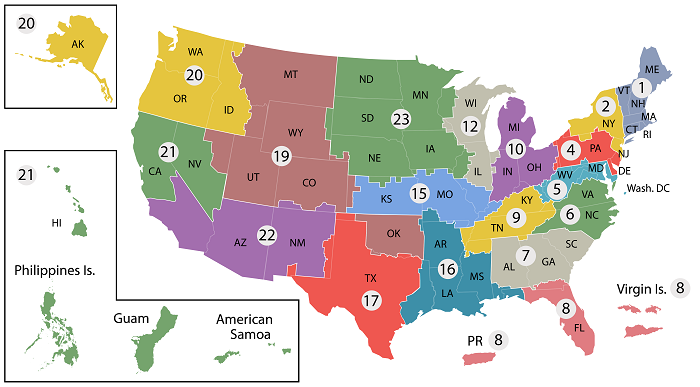
- VISN 1: VA New England Healthcare System
- VISN 2: New York/New Jersey VA Health Care Network
- VISN 4: VA Healthcare - VISN 4
- VISN 5: VA Capitol Health Care Network
- VISN 6: VA Mid-Atlantic Health Care Network
- VISN 7: VA Southeast Network
- VISN 8: VA Sunshine Healthcare Network
- VISN 9: VA MidSouth Healthcare Network
- VISN 10: VA Healthcare System
- VISN 12: VA Great Lakes Health Care System
- VISN 15: VA Heartland Network
- VISN 16: South Central VA Health Care Network
- VISN 17: VA Heart of Texas Health Care Network
- VISN 19: Rocky Mountain Network
- VISN 20: Northwest Network
- VISN 21: Sierra Pacific Network
- VISN 22: Desert Pacific Healthcare Network
- VISN 23: VA Midwest Health Care Network




















