MIRECC / CoE
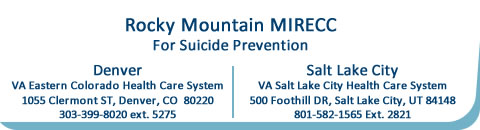
Rocky Mountain MIRECC for Veteran Suicide Prevention

Updated: 6 December 2018
Biography
- Jeri E. Forster PhD
 Title: Rocky Mountain MIRECC Data and Statistical Core Director
Title: Rocky Mountain MIRECC Data and Statistical Core Director- Contact information:
720.938.2708
Jeri.Forster@ucdenver.edu - Dr. Jeri Forster obtained a PhD in Biostatistics from the University of Colorado Health Sciences Center in 2006. She began work as a faculty member of the Department of Pediatrics, School of Medicine, University of Colorado Denver in the 2006, with a secondary appointment in the Department of Biostatistics and Informatics. In 2007, Dr. Forster began providing biostatistical consulting to the Denver VA Medical Center Mental Illness, Research, Education and Clinical Center (MIRECC) on a number of projects and studies related to TBI, PTSD and suicide risk. This collaboration grew over the next 5 years and Dr. Forster joined the Rocky Mountain MIRECC team as the Director of the newly formed Data and Statistical Core (DASC) in 2012.
- Her contributions include: Coordinating and building the infrastructure of the DASC with its members; continuing the growth of the DASC through strategic planning with the group; serving as Co-Investigator on multiple projects; providing expert consultation on study design, hypothesis refinement, and statistical considerations on numerous projects; and aiding in development of presentations and manuscripts with input on results, interpretation, graphs, tables, and statistical analysis descriptions. Dr. Forster has mentored junior investigators who wish to perform analyses for their projects and provided Post Doctoral Fellows with more in-depth mentoring regarding project development from a statistical perspective. Additionally, Dr. Forster serves on the Research Oversight Committee at the MIRECC which reviews all MIRECC projects. Lastly, she maintains an academic appointment as Assistant Clinical Professor at the University Of Colorado School Of Medicine, Department of Physical Medicine and Rehabilitation and in the Colorado School of Public Health, Department of Biostatistics and Informatics.
- Research Interests: Longitudinal data analysis; nonignorable dropout; varying-coefficient models
- Statement about Research Program: My research has focused on methods that adjust for potential nonignorable dropout in longitudinal observational studies and clinical trials. I have additionally led analyses on numerous studies related to TBI, PTSD and suicide risk.
- Available Project(s) for Fellows: n/a
Recent Publications
Barnes SM, Monteith LL, Forster JE, Nazem S, Borges LM, Stearns-Yoder KA, Bahraini NH. Developing Predictive Models to Enhance Clinician Prediction of Suicide Attempts Among Veterans With and Without PTSD. Suicide Life Threat Behav. 2018 Sep 11. doi: 10.1111/sltb.12511. [Epub ahead of print] PubMed PMID: 30206955.
Barnes, S.M., Monteith, L.L., Forster, J.E., Nazem, S., Borges, L.M., Stearns-Yoder, K.A., & Bahraini, N.H. (2018). Developing predictive models to enhance clinician prediction of suicide attempts among veterans with and without PTSD. Suicide and Life-Threatening Behavior. https://doi.org/10.1111/sltb.12511
Persistent Symptoms and Objectively Measured Balance Performance Among OEF/OIF Veterans With Remote Mild Traumatic Brain Injury
27 February 2018 - RMIRECC authors Jeri Forster PhD, Kelly Stearns-Yoder MA, and Lisa Brenner PhD participated in writing this paper along with colleagues from the University of Colorado School of Medicine, Physical Medicine and Rehabilitation Department. This study explored the relationships between dizziness, fatigue, and depression and PTSD and balance in Veterans with mTBI. "Findings suggest that dizziness, fatigue, depression and PTSD, and time since most recent mTBI may influence balance performance." Read more
Fogleman ND, Naaz F, Knight LK, Stoica T, Patton SC, Olson-Madden JH, Barnhart MC, Hostetter TA, Forster J, Brenner LA, Banich MT, Depue BE. Reduced lateral prefrontal cortical volume is associated with performance on the modified Iowa Gambling Task: A surface based morphometric analysis of previously deployed veterans. Psychiatry Res. 2017 Jun 28;267:1-8. doi: 10.1016/j.pscychresns.2017.06.014.
Bahraini, N.H., Monteith, L.L., Gerber, H.R., Forster, J.E., Hostetter, T.A., & Brenner, L.A. (2017). The Association Between Posttraumatic Stress Disorder and Perceptions of Deployment-Related Injury in Veterans With and Without Mild Traumatic Brain Injury. Journal of Head Trauma Rehabilitation. doi: 10.1097/HTR.0000000000000307.
Monteith, L.L., Bahraini, N.B., Matarazzo, B.B., Gerber, H., Soberay, K.A., & Forster, J.E. (2016). The Influence of Gender on Suicidal Ideation following Military Sexual Trauma among Veterans in the Veterans Health Administration. Psychiatry Research, July, doi:10.1016/j.psychres.2016.07.036
Barnes, S. M., Bahraini, N. H., Forster, J. E., Stearns-Yoder, K. A., Hostetter, T. A., Smith, G., Nagamoto, H. T. and Nock, M. K. (2016), Moving Beyond Self-Report: Implicit Associations about Death/Life Prospectively Predict Suicidal Behavior among Veterans. Suicide and Life-Threat Behavi. doi: 10.1111/sltb.12265
Moore CM, MaWhinney S, Forster JE, Carlson NE, Allshouse A, Wang X, Routy JP, Conway B, Connick E. Accounting for dropout reason in longitudinal studies with nonignorable dropout. Stat Methods Med Res. 2015 Jun 15. pii: 0962280215590432. [Epub ahead of print]
Forster JE, MaWhinney S, Ball E, and Fairclough D. (2012) A varying-coefficient method for analyzing longitudinal clinical trials data with nonignorable dropout. Contemporary Clinical Trials, 33:378-85.
Barnes SM, Russell LM, Hostetter TA, Forster JE, Devore MD, Brenner LA. (2015) Characteristics of traumatic brain injuries sustained among Veterans seeking homeless services. Journal of Health Care for the Poor and Underserved, 26(1):92-105. PMID:2570273
Olson-Madden J, Homaifar BY, Nagamoto H, Schneider AL, Forster J, Matarazzo BE, Bogner JA, Corrigan JD, Brenner LA, and Hostetter TA. (2014) Validating the Traumatic Brain Injury-4 (TBI-4) screening measure for Veterans seeking mental health treatment with psychiatric inpatient and outpatient service utilization. Archives of Physical Medicine and Rehabilitation, 95(5):925-9.
Lampe E, Forster J, Herbst E, Spitz M, and Frey L. (2014) Pre-admission clinical factors affect length of stay in epilepsy monitoring unit. Neurodiagnostic Journal, 54(2):138-47. PMID: 25080773
Rings JA, Gutierrez PM, and Forster JE. (2014) Exploring prolonged grief symptomology and its relationship to suicide risk among Veterans. Military Behavioral Health, 2(3):283-292
Betthauser LM, Brenner LA, Forster JE, Hostetter TA, Schneider AL, and Hernandez TH. (2014) A factor analysis and exploration of attitudes and beliefs towards complementary and conventional medicine in Veterans. Medical Care, 52(12 Suppl 5):S50-6. PMID:25397824
Grants
- Military Suicide Research Consortium
- A novel approach to identifying behavioral and neural markers of active suicidal ideation: Effects of cognitive and emotional stress on working memory in OEF/OIF/OND Veterans. Role: Co-Investigator
- Military Suicide Research Consortium
- Home-Based Mental Health Evaluation (HOME) to Assist Suicidal Veterans with the Transition from Inpatient to Outpatient Settings: A Multi-Site Interventional Trial. Role: Co-Investigator