MIRECC / CoE
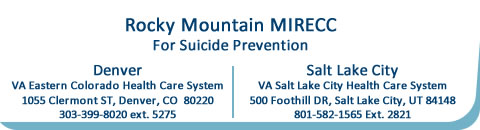
Rocky Mountain MIRECC for Veteran Suicide Prevention

Updated: 4 November 2019
Biography
- Bridget B. Matarazzo, PsyD
 Title: Director for Clinical Services
Title: Director for Clinical Services
Clinical/Research Psychologist- Contact:
720-256-1868
bridget.matarazzo@va.gov -
Fellowship Training Faculty
Accepting fellowship applications for 2021- Clinical Interest:
Suicide risk assessment and management; dissemination and implementation of evidence-based suicide prevention interventions and clinical practice guidelines’ supporting providers who support Veterans at risk for suicide - Year of Licensure: 2011
- Biography:
Dr. Bridget Matarazzo is a Clinical Research Psychologist and the Director of Clinical Services at VA’s Rocky Mountain MIRECC for Suicide Prevention and an Associate Professor in the Department of Psychiatry at the University of Colorado School of Medicine. She completed her Pre-Doctoral Internship at the Denver VA Medical Center and obtained a PsyD in Clinical Psychology from the University of Denver in 2010. She is a licensed clinical psychologist in the state of Colorado.Dr. Matarazzo is passionate about applying implementation science research to promote the dissemination and implementation of evidence-based suicide prevention strategies to enhance care for Veterans. She partners closely with colleagues in the VA Office of Mental Health and Suicide Prevention to develop and implement national suicide programs and initiatives. Her team uses evidence-based implementation strategies to provide technical assistance, training and quality assurance/improvement to support these programs. One such project is VA’s Suicide Risk Identification Strategy (Risk ID), which is the nation’s largest population-based screening and evaluation initiative. Another is VA’s REACH VET program, which utilizes predictive analytics to identify and support Veterans at increased risk for suicide. Her research focuses on evaluation of these implementation strategies and programmatic evaluation of these initiatives (e.g., Co-Investigator on Dr. Nazanin Bahraini’s QUERI Partnered Evaluation Initiative aimed and developing and examining an adaptive implementation strategy to improve uptake of Risk ID in ambulatory care settings).
Dr. Matarazzo’s research interests also relate to engaging Veterans in care, particularly during high-risk transitions in care. For example, she was the Principal Investigator of a Military Suicide Research Consortium-funded multi-site interventional trial aimed at studying the effectiveness of the Home-Based Mental Health Evaluation (HOME) Program, which she developed with her colleagues in the Rocky Mountain MIRECC. She now consults with staff at multiple VA facilities that have implemented the HOME Program.
Additionally, Dr. Matarazzo is deeply committed to supporting providers who deliver suicide prevention care to Veterans. She is Co-Director of VA’s Suicide Risk Management Consultation Program, which supports VA and community providers serving Veterans at risk for suicide. Her team provides consultation, resources and training to support those doing such incredibly important work. #NeverWorryAlone
Dr. Matarazzo’s clinical interests are in suicide risk assessment and management for Veterans at high risk for suicide and PTSD treatment as a certified Cognitive Processing Therapy provider. She is also a member of the Rocky Mountain MIRECC Training Committee and provides supervision to Post-Doctoral Fellows and Psychology Interns.
Fellowship Applications: Dr. Matarazzo is accepting fellowship applications for 2021. Applicants with an interest in evaluating patient and provider perspectives as they relate to VA national suicide prevention programs as well programmatic evaluation of these programs are encouraged to apply. Fellows could be involved in current projects or propose secondary projects that may augment existing projects. Please email Dr. Matarazzo for more details or to set up a time to discuss potential projects and research alignment prior to applying.
- Statement about Research Program: Statement about Research Program: Dr. Matarazzo’s research primarily focuses on the development and examination of clinical interventions to help engage Veterans in care and decrease suicide risk among Veterans. Her main line of research is related to the Home-Based Mental Health HOME Program, which aims to engage Veterans in care and mitigate suicide risk during the high-risk period following psychiatric hospitalization. She is currently the Principal Investigator of a multi-site clinical trial examining the effectiveness of the HOME program. Additionally, she is examining implementation and effectiveness of implementing the HOME program with rural Veterans. Finally, she conducts program evaluation of the National Suicide Risk Management Consultation Program and REACH VET program.
Recent Publications
- Publication: Therapeutic Risk Management: Chain Analysis of Suicidal Ideation and Behavior
- 1 April 2019 - RMIRECC PIs Lauren Borges, PhD, Sarra Nazem, PhD, Bridget Matarazzo, PsyD, Sean Barnes, PhD, and Hal Wortzel, MD write "Structural approaches to suicide risk assessment (eg, evaluating the frequency and intensity of suicidal ideation and classifying types of suicidal behavior) often fall short of providing an idiographic and dynamic analysis of the factors driving and maintaining an individual's suicide risk. Structural approaches can be bolstered through chain analysis which facilitates an exploration of the factors maintaining suicidal ideation and behavior based on positive and negative reinforcement. By uncovering the factors causing suicidal ideation and behavior to persist, efficient intervention strategies can be selected to target these pathways. In this column, the authors delineate the use of chain analysis to guide suicide risk assessment and inform treatment planning." Read more
- Monteith, L. L., Bahraini, N. H., Gerber, H. R., Dorsey Holliman, B., Schneider, A. L., Holliday, R., & Matarazzo, B. B. (2018). Military sexual trauma survivors’ perceptions of veterans health administration care: A qualitative examination. Psychological Services. Advance online publication. http://dx.doi.org/10.1037/ser0000290
- Although the Veterans Health Administration (VHA) provides free health care related to military sexual trauma (MST), many veterans forgo or delay such care, underscoring the need for research aimed at understanding MST survivors’ perceptions and concerns regarding VHA care. This study employed a qualitative phenomenological approach to describe MST survivors’: (a) perceptions of VHA care, (b) concerns about VHA care, and (c) suggestions for how VHA can facilitate recovery from MST. Fifty veterans (32 women, 18 men) with histories of MST participated in semistructured interviews. Transcripts were analyzed using thematic analysis. The pattern of themes was examined by gender and MST type. The majority of participants described neutral or positive perceptions of VHA care; however, a subset of participants described negative perceptions and reservations about using VHA care. Participants expressed concerns regarding distrust, provider compassion, privacy, stigma, shame, and continuity of care. Some women, particularly those who experienced military sexual assault, also described gender-related distress (e.g., feeling anxious or out of place, desire for separate facilities). Both men and women described wanting nonspecific support, improved continuity of care, and the ability to choose from a variety of treatment options (e.g., holistic, gender-specific). Further research is needed to examine if these findings are replicated in other samples. (PsycINFO Database Record (c) 2018 APA, all rights reserved)
- Petrik, M.L., Miller, B.F. & Matarazzo, B. (2017). Factors influencing suicide risk assessment and management in VA primary care clinics: A qualitative study of provider perspectives. Military Behavioral Health. DOI: 10.1080/21635781.2017.1379452
- This study obtained the perspectives of 11 providers employed in Veteran Affairs (VA) primary care clinics across 4 states regarding the factors that influence the assessment and management of suicide risk. Qualitative data was analyzed using a hybrid inductive-deductive thematic analysis approach. Themes highlighted the impact of a trusting patient–provider relationship, multidisciplinary team-based care, education about suicide prevention from integrated behavioral health providers, reliable access to mental health care, and VA system-wide suicide prevention efforts in supporting generalists' ability to effectively assess and manage veterans' suicide. Recommendations for enhancing evidence-based care for suicide risk in primary care are discussed. KEYWORDS: Veterans, suicide, assessment, management, primary care, qualitative research
- Brenner LA, Homaifar BY, Olson-Madden JH, Nagamoto HT, Huggins J, Schneider AL, Forster JE, Matarazzo B, Corrigan JD. Prevalence and Screening of Traumatic Brain Injury Among Veterans Seeking Mental Health Services. J Head Trauma Rehabil. 2013 Jan;28(1):21-30.
 OBJECTIVES:: To assess the prevalence of traumatic brain injury (TBI) among Veterans seeking mental health services using a 4-item tool, the Traumatic Brain Injury-4 (TBI-4), and to establish the classification accuracy of the TBI-4 using the Ohio State University TBI-Identification Method as the criterion standard. STUDY DESIGN:: Archival and observational data collected from individuals seeking care at a Mountain State VA Medical Center. PARTICIPANTS:: The sample for the archival study was 1810. Three hundred sixteen Veterans completed observational study measures. MAIN MEASURES:: For the archival study, TBI-4 and demographic data extracted from electronic medical records. For the observational study, the Ohio State University TBI-Identification Method and a demographic questionnaire were used. TBI-4 data were also obtained from electronic medical records. RESULTS:: The prevalence of probable TBI among those seeking VA MH treatment was 45%. Sensitivity and specificity of the TBI-4 were 0.74 and 0.56, respectively. Veterans with all levels of TBI severity sought care within this VA mental health setting. CONCLUSIONS:: The prevalence of TBI in this VA mental health treatment population was higher than expected. Additional research is required to assess the clinical utility of screening for TBI among this population of Veterans.
OBJECTIVES:: To assess the prevalence of traumatic brain injury (TBI) among Veterans seeking mental health services using a 4-item tool, the Traumatic Brain Injury-4 (TBI-4), and to establish the classification accuracy of the TBI-4 using the Ohio State University TBI-Identification Method as the criterion standard. STUDY DESIGN:: Archival and observational data collected from individuals seeking care at a Mountain State VA Medical Center. PARTICIPANTS:: The sample for the archival study was 1810. Three hundred sixteen Veterans completed observational study measures. MAIN MEASURES:: For the archival study, TBI-4 and demographic data extracted from electronic medical records. For the observational study, the Ohio State University TBI-Identification Method and a demographic questionnaire were used. TBI-4 data were also obtained from electronic medical records. RESULTS:: The prevalence of probable TBI among those seeking VA MH treatment was 45%. Sensitivity and specificity of the TBI-4 were 0.74 and 0.56, respectively. Veterans with all levels of TBI severity sought care within this VA mental health setting. CONCLUSIONS:: The prevalence of TBI in this VA mental health treatment population was higher than expected. Additional research is required to assess the clinical utility of screening for TBI among this population of Veterans.- Keywords: Assessment, Suicide Prevention, Traumatic Brain Injury (TBI)
- Return to Top
- Homaifar B, Matarazzo B, Wortzel HS. Therapeutic risk management of the suicidal patient: augmenting clinical suicide risk assessment with structured instruments. J Psychiatr Pract. 2013 Sep;19(5):406-9.
- This column is the second in a series presenting a model for therapeutic risk management of the suicidal patient. As discussed in the first part of the series, the model involves several elements including augmenting clinical risk assessment with structured instruments, stratifying risk in terms of both severity and temporality, and developing and documenting a safety plan. This column explores in more detail how to augment clinical risk assessment with structured instruments. Unstructured clinical interviews have the potential to miss important aspects of suicide risk assessment. By augmenting the free-form clinical interview with structured instruments that demonstrate reliability and validity, a more nuanced and multifaceted approach to suicide risk assessment is achieved. Incorporating structured instruments into practice also serves a medicolegal function, since these instruments may become a living part of the medical record, establishing baseline levels of suicidal thoughts and behaviors and facilitating future clinical determinations regarding safety needs. We describe several instruments used in a multidisciplinary suicide consultation service, each of which has demonstrated relevance to suicide risk assessment and screening, ease of administration, and strong psychometric properties. In addition, we emphasize the importance of viewing suicide risk assessment as an ongoing process rather than as a singular event. Finally, we discuss special considerations in the evolving practice of risk assessment. (Journal of Psychiatric Practice 2013;19:406-409).
- Keywords: Suicide Prevention
- Return to Top
- Matarazzo BB, Barnes SM, Pease JL, Russell LM, Hanson JE, Soberay KA, Gutierrez PM. Suicide Risk among Lesbian, Gay, Bisexual, and Transgender Military Personnel and Veterans: What Does the Literature Tell Us? Suicide Life Threat Behav. 2014 Feb 3.
- Research suggests that both the military and veteran and the lesbian, gay, bisexual, and transgender (LGBT) populations may be at increased risk for suicide. A literature review was conducted to identify research related to suicide risk in the LGBT military and veteran populations. Despite the paucity of research directly addressing this issue, themes are discussed evident in the literature on LGBT identity and suicide risk as well as LGBT military service members and veterans. Factors such as social support and victimization appear to be particularly relevant. Suggestions are made with respect to future research that is needed on this very important and timely topic. © Published 2014. This article is a U.S. Government work and is in the public domain in the USA.
- Keywords: Suicide Prevention
- Matarazzo, B. B., Clemans, T. A., Silverman, M. M., & Brenner, L. A. (2013). The Self-Directed Violence Classification System and the Columbia Classification Algorithm for Suicide Assessment: A crosswalk. Suicide and Life-Threatening Behavior, 43, 235-249.
- The lack of a standardized nomenclature for suicide-related thoughts and behaviors prompted the Centers for Disease Control and Prevention, with the Veterans Integrated Service Network 19 Mental Illness Research Education and Clinical Center, to create the Self-Directed Violence Classification System (SDVCS). SDVCS has been adopted by the Department of Veterans Affairs and the Department of Defense. Another classification system, the Columbia Classification Algorithm for Suicide Assessment, has been recommended by the Food and Drug Administration. To facilitate the use of both systems, this article provides a "crosswalk" between the two classification systems.
- Keywords: Suicide Prevention
- Return to Top
- Matarazzo BB, Hoffberg AS, Clemans TA, Signoracci GM, Simpson GK, Brenner LA. Cross-cultural adaptation of the Window to Hope: A psychological intervention to reduce hopelessness among US Veterans with traumatic brain injury. Brain Inj. 2014 Jun 19:1-10.
- Abstract Primary objective: To conduct a cross-cultural adaptation of Window to Hope (WtoH), a treatment to reduce hopelessness after traumatic brain injury (TBI), from the Australian civilian context to that of US Veterans. Research design: Three-stage mixed-methods approach. Methods: Stage 1: Consensus conference with stakeholders to revise the manual. Stage 2: Pilot study of the revised manual with US Veterans to examine acceptability, feasibility and fidelity. Stage 3: Review of results with consensus conference attendees and further revisions. Results: Stage 1: Conference attendees reached 100% consensus regarding changes made to the manual. Stage 2: Qualitative results yielded themes that suggest that participants benefitted from the intervention and that multiple factors contributed to successful implementation (Narrative Evaluation of Intervention Interview, User Feedback Survey-Modified, Post-Treatment Interviews). Therapists achieved 100% treatment fidelity. Quantitative results from the Client Satisfaction Questionnaire-8 suggest that the intervention was acceptable. Stage 3: The culturally adapted manual was finalized. Conclusions: Results of this study suggest that the revised WtoH manual is acceptable and feasible. US therapists exhibited adherence to the protocol. The three-stage methodology was successfully employed to cross-culturally adapt an intervention that is well-suited for a Phase II randomized controlled trial among US military Veterans.
- Pubmed Keywords: Cognitive behaviour therapy; mental health; suicide prevention
- Return to Top
- Matarazzo BB, Homaifar BY, Wortzel HS. Therapeutic risk management of the suicidal patient: safety planning. J Psychiatr Pract. 2014 May;20(3):220-4.
- This column is the fourth in a series describing a model for therapeutic risk management of the suicidal patient. Previous columns presented an overview of the therapeutic risk management model, provided recommendations for how to augment risk assessment using structured assessments, and discussed the importance of risk stratification in terms of both severity and temporality. This final column in the series discusses the safety planning intervention as a critical component of therapeutic risk management of suicide risk. We first present concerns related to the relatively common practice of using no-suicide contracts to manage risk. We then present the safety planning intervention as an alternative approach and provide recommendations for how to use this innovative strategy to therapeutically mitigate risk in the suicidal patient. (Journal of Psychiatric Practice 2014;20:220-224).
- Keywords: Suicide Prevention
- Return to Top
- Monteith, L.L., Bahraini, N.B., Matarazzo, B.B., Gerber, H., Soberay, K.A., & Forster, J.E. (2016). The Influence of Gender on Suicidal Ideation following Military Sexual Trauma among Veterans in the Veterans Health Administration. Psychiatry Research, July, doi:10.1016/j.psychres.2016.07.036
- No studies have examined whether military sexual trauma, as measured and defined within the Veterans Health Administration (VHA), is associated with suicidal ideation among Veterans in VHA care, when taking prior suicide attempts into account. Research regarding the role of gender in this association is also limited. The present study examined: (1) whether military sexual trauma was associated with the presence of past-week suicidal ideation among 354 Veterans in VHA (310 men, 44 women); (2) whether gender moderated the association between military sexual trauma and suicidal ideation. Information regarding military sexual trauma, suicidal ideation, suicide attempt, and psychiatric diagnoses was obtained from self-report instruments and medical records. Adjusting for age, gender, combat, posttraumatic stress disorder, depressive disorders, negative affect, and lifetime suicide attempt, Veterans with military sexual trauma were significantly more likely to report suicidal ideation, compared to Veterans without military sexual trauma. Furthermore, the association between military sexual trauma and suicidal ideation was stronger for men compared to women. These results contribute to a growing literature identifying military sexual trauma as a risk factor for suicidal thoughts and behaviors among Veterans in VHA care and emphasize the importance of screening for suicidal ideation among survivors of military sexual trauma.
- Keywords: Suicide Prevention, Military Sexual Trauma
- Return to Top
- Olson-Madden JH, Brenner LA, Matarazzo BB, Signoracci GM; Expert Consensus Collaborators. Identification and Treatment of TBI and Co-occurring Psychiatric Symptoms Among OEF/OIF/OND Veterans Seeking Mental Health Services Within the State of Colorado: Establishing Consensus for Best Practices. Community Ment Health J. 2013 Jan 17. [Epub ahead of print]
- This paper highlights the results of a consensus meeting regarding best practices for the assessment and treatment of co-occurring traumatic brain injury (TBI) and mental health (MH) problems among Operation Enduring Freedom/Operation Iraqi Freedom/Operation New Dawn Veterans seeking care in non-Veterans Affairs Colorado community MH settings. Twenty individuals with expertise in TBI screening, assessment, and intervention, as well as the state MH system, convened to establish and review questions and assumptions regarding care for this Veteran population. Unanimous consensus regarding best practices was achieved. Recommendations for improving care for Veterans seeking care in community MH settings are provided.
- Keywords: Assessment, OEF/OIF/OND, Traumatic Brain Injury (TBI)
- Return to Top
- Olson-Madden JH, Homaifar BY, Hostetter T, Matarazzo BB, Huggins J, Forster JE, Schneider AL, Nagamoto HT, Corrigan JD, Brenner LA. Validating the Traumatic Brain Injury-4 (TBI-4) Screening Measure for Veterans Seeking Mental Health Treatment with Psychiatric Inpatient and Outpatient Service Utilization Data. Arch Phys Med Rehabil. 2014 Jan 27.
- OBJECTIVE: To determine whether a positive screen on the Traumatic Brain Injury-4 (TBI-4) can identify Veterans who utilize more inpatient and outpatient mental health services. Two criteria to identify a positive screen were evaluated. DESIGN: Validation cohort. SETTING: Veterans Affairs Medical Center. PARTICIPANTS: Individual seeking Veterans Health Administration mental health services (N=1,493). INTERVENTIONS: Not applicable. MAIN OUTCOME MEASURES: One year of inpatient and outpatient mental health utilization data following the TBI-4 screen date. RESULTS: In the year post-mental health intake, those who answered positively to any of the four TBI-4 screening questions (Criterion 1) or Question 2 (Criterion 2; ever being "knocked out") had significantly more psychiatric hospitalizations compared to those who met neither criterion. Those who were positive by Criterion 2 also had significantly fewer outpatient mental health contacts. CONCLUSIONS: Veterans screening positive for history of TBI on the TBI-4 had more hospital stays in the year post-mental health intake. Those who reported having been "knocked out", also had fewer outpatient mental health visits. These findings may suggest an overall relationship in this population between greater needs for mental health care and likelihood of prior injury. For those with a history of loss of consciousness, the reduced use of outpatient care may reflect greater problems engaging in treatment or with preventive aspects of the healthcare system, when they are not in crisis. Using a screener such as the TBI-4 could facilitate identification of Veterans who might benefit from targeted and intensive outpatient interventions to avoid frequent inpatient psychiatric hospitalization. Copyright © 2014 American Congress of Rehabilitation Medicine. Published by Elsevier Inc. All rights reserved.
- PubMed Keywords: (CDW), (CPT), (TBI), (TBI-4), (TBI-ID), (VAMC), (VHA), Corporate Data Warehouse, Current Procedural Terminology, Traumatic Brian Injury-Identification, Traumatic brain injury, Veterans Administration Medical Center, Veterans Health Administration, hospitalization, mental health, the Traumatic Brain Injury-4, traumatic brain injury, utilization
- Wortzel HS, Homaifar B, Matarazzo B, Brenner LA. Therapeutic risk management of the suicidal patient: stratifying risk in terms of severity and temporality. J Psychiatr Pract. 2014 Jan;20(1):63-7.
- This column is the third in a series describing a model for therapeutic risk management of the suicidal patient. In the preceding column, we described augmenting clinical suicide risk assessment with structured instruments. In this column, we describe how clinicians can use the totality of available clinical data to offer a two-dimensional risk stratification that qualifies risk in terms of both severity and temporality. By offering two separate designations that reflect severity for both acute and chronic risk, conceptualizing and communicating a patient's risk for suicide is accomplished in a more nuanced way, providing the level of detail necessary when working with high risk individuals, especially those struggling with chronic suicidal ideation. Formulations reflecting suicide risk need to be accurate and facilitate good clinical decision-making in order to optimally balance the principles of autonomy, non-maleficence, and beneficence. Stratifying risk in terms of both severity and temporality helps identify situations in which involuntary hospitalization is warranted, while also helping to minimize unnecessary admissions. Hence, two-dimensional risk stratification that addresses both acute and chronic risk for suicide is an essential component of therapeutic risk management of the suicidal patient.
- Keywords: Suicide Prevention
- Wortzel HS, Matarazzo B, Homaifar B. A model for therapeutic risk management of the suicidal patient. J Psychiatr Pract. 2013 Jul;19(4):323-6.
- While the practice of psychiatry involves many challenges, few scenarios are as clinically and emotionally demanding as managing the patient who is at high risk for suicide. Risk management is a reality of psychiatric practice, and this necessitates practicing and documenting thoughtful suicide risk assessment and management. Therapeutic risk management is based on clinical risk management that is patient-centered, supportive of the treatment process, and maintains the therapeutic alliance. In this article, the authors present a broad overview of a model for achieving therapeutic risk management of the suicidal patient that involves augmenting clinical risk assessment with structured instruments, stratifying risk in terms of both severity and temporality, and developing and documenting a safety plan. These elements are readily accessible to and deployable by mental health clinicians in most disciplines and treatment settings, and they collectively yield a suicide risk assessment and management process (and attendant documentation) that should withstand the scrutiny that often occurs in the wake of a patient suicide or suicide attempt. (Journal of Psychiatric Practice 2013;19:323-326).
- Keywords: Suicide Prevention
Presentations
Grants/Funding
- Home-Based Mental Health Evaluation (HOME): A Multi-Site Trial
 Department of Defense
Department of Defense- Window to Hope – Evaluating a Psychological Treatment for Hopelessness among Veterans with Traumatic Brain Injury and Problem Solving Therapy for Suicide Prevention Among Veterans with TBI
 Department of Defense
Department of Defense- Increasing Statewide Capacity to Provide Mental Health Care to Eligible Operation Enduring Freedom (OEF)/Operation Iraqi Freedom (OIF) Veterans with TBI and Co-Occurring Behavioral Health Issues
 Health Resources and Services Administration (HRSA)
Health Resources and Services Administration (HRSA)- Home-Based Mental Health Evaluation: A Model for Assisting Suicidal Veterans with the Transition form Inpatient to home
 Veterans Administration
Veterans Administration