About CPG
What is a CPG?
Clinical Practice Guidelines contain research informed recommendations on how to diagnose and treat a medical or psychiatric condition. This site explores the CPG for Patients at Risk for Suicide.
What is the VA/DoD Clinical Practice Guideline for Patients at Risk for Suicide?
The VA/DoD CPG for Patients at Risk for Suicide uses evidence-based information to guide health care providers in screening, evaluation, treatment, and case management. It provides clinical practice recommendations for the care of service members and Veterans at risk for suicide, as well as guidance to inform specialty referrals.
How can this site help apply the CPG's recommendations in practice?
This site helps translate the recommendations into tangible strategies by providing a roadmap and resources for how to apply them to the service members and Veterans you serve.
Who should use this CPG?
This CPG is intended for use by Department of Veterans Affairs (VA) and Department of Defense (DoD) health care practitioners and those in the community involved in the care of service members or Veterans at risk for suicide.
What’s changed in the revised 2024 CPG?
The 2024 CPG is an update to the 2019 CPG. It contains the following significant revisions:
- Updated Algorithm
- Reviewed studies focused on specific outcomes to include critical outcomes of suicide attempt and suicide death
- Added eight new recommendations; 12 reviewed and replaced, 3 amended, and 1 no change
- Used more rigorous application of GRADE methodology
- Updated Routine Care for Suicide Prevention section
- Updated Research Priorities section
Note: Recommendation strength downgrades from Weak for to Neither for nor against do not imply that providers should avoid these options, rather that the data from the systematic evidence review is insufficient to make a recommendation when using more rigorous methodology.
To learn more, check out the lecture What’s Changed in the 2024 Revised CPG for Suicide Prevention? presented by Drs. Bridget Matarazzo & Hal Wortzel.
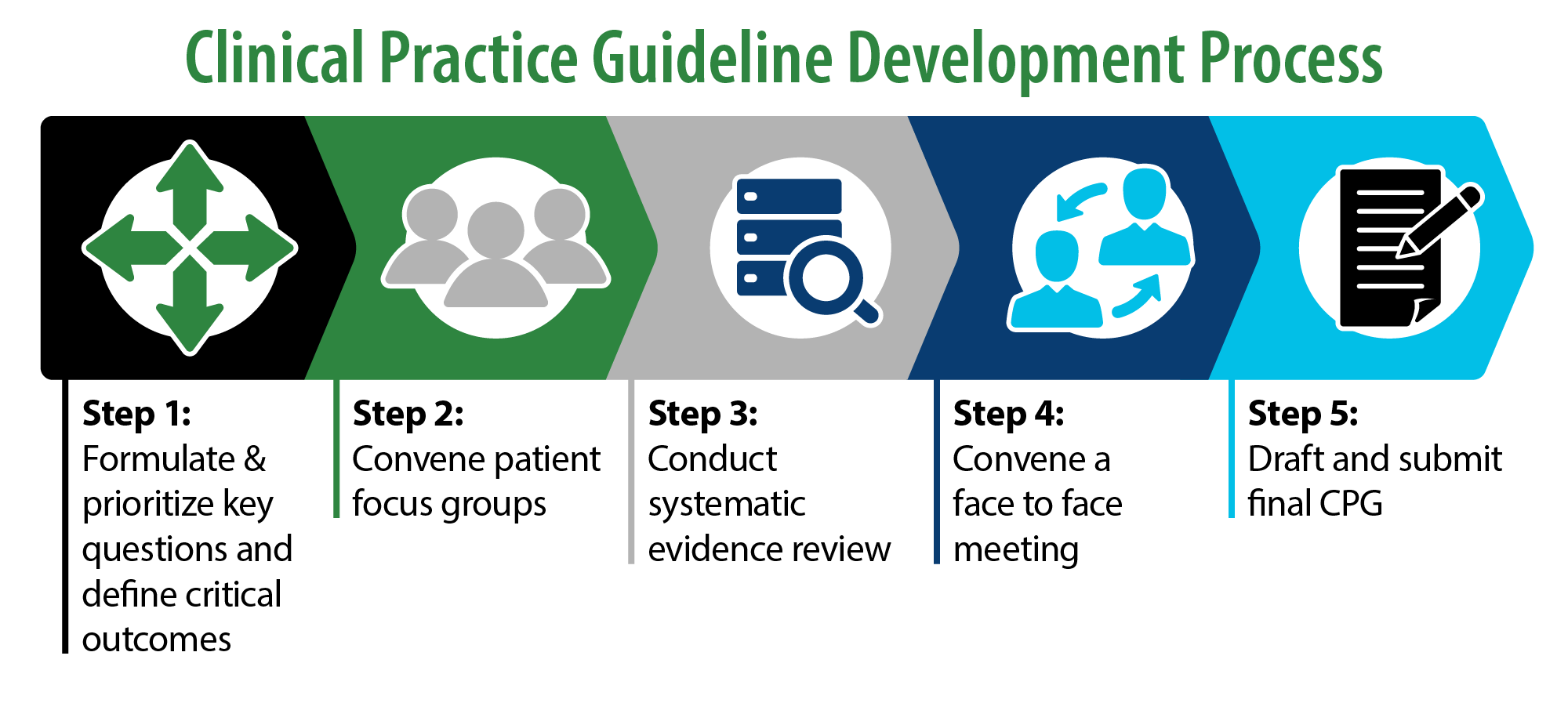
How was the CPG for Patients at Risk for Suicide developed?
The VA/DoD CPG for Patients at Risk for Suicide is based on a systematic review of both clinical and epidemiological evidence. Developed by a panel of multidisciplinary experts in VA and DoD, it provides a review of relevant literature that informs each recommendation. The CPG also rates the quality of the evidence and the strength for each of the 22 recommendations.
Level of Evidence
Each recommendation is graded by assessing the quality of the overall evidence base, the associated benefits and harms, patient and provider values and preferences, and other implications of the recommendation. Specifically, the GRADE (Grading of Recommendations Assessment, Development and Evaluation) approach was used by VA and DoD Evidence-Based Practice Work Group (EBPWG) to develop this CPG and corresponding recommendations.
Recommendation Category

The evidence for each recommendation was reviewed. Then, based on this evidence review, each recommendation was categorized as:
- "New-added"
- "New-replaced"
- "Not changed"
- "Amended"
- "Deleted"
Recommendation Strength

The grade of each recommendation is presented as part of a continuum:
- Strong For (or "We recommend offering this option …")
- Weak For (or "We suggest offering this option …")
- No recommendation for or against (or "There is insufficient evidence …")
- Weak Against (or "We suggest not offering this option …")
- Strong Against (or "We recommend against offering this option …")




















