MIRECC Presents Archive 2019-2020
MIRECC Presents Archive
June 3, 2020: Posttraumatic headaches: Current concepts in pathophysiology, diagnosis, and management
Cynthia Mayer, DO
Chronic headaches can occur after trauma and can co-exist with traumatic brain injury and chronic PTSD, causing significant discomfort for patients and impairing optimal functioning. This presentation will summarize the current status of clinical care and research related to posttraumatic headaches and discuss guidelines for assessment and treatment.
April 15, 2020: The role of religion/spirituality in mental health outcomes for PTSD
Zhen Cheng, PhD
Religion and spirituality have become increasingly important in psychiatric assessment and treatment. They can be an important part of cultural heritage, and they also can be important in healing and social supports. This presentation discussED the relevance of religion and spirituality in clinical outcomes for mental health conditions, including PTSD.
April 1, 2020: Treatment engagement and retention in patients with PTSD
Shannon Kehle-Forbes, PhD
Despite the development of evidence-based, effective treatments for PTSD within VA, treatment engagement and retention continue to be challenging, but they are essential for effective treatment. This presentation will explore some of the factors that influence engagement and retention and provide clinical suggestions for optimizing treatment engagement and retention.
Alzheimer’s Disease continues to be an important contributor to morbidity and mortality among Veterans. The glymphatic system, a brain-wide network that facilitates the clearance of waste products, has been demonstrated to fail in the aging brain and in the young brain after traumatic brain injury. Impairment of glymphatic function may link brain trauma early in life with the development of dementia in later years. This clinically relevant presentation will explore the implications of impairment of glymphatic function for vulnerability to Alzheimer’s Disease.
March 4, 2020: Dialectical Behavioral Therapy (DBT) for treating PTSD
Melanie S. Harned, PhD, ABPP
Dialectical Behavior Therapy (DBT) was originally developed to treat chronically suicidal and self-injuring individuals with multiple mental disorders and pervasive emotion dysregulation. From its inception, DBT has highlighted the role of trauma as a common etiological factor and posttraumatic stress disorder (PTSD) as an important treatment target for many patients who receive this treatment. In this talk, the basic structure and procedures of the DBT Prolonged Exposure (DBT PE) protocol will be outlined and the clinical challenges encountered during its development will be discussed. In addition, research findings supporting the safety and effectiveness of the integrated DBT and DBT PE protocol treatment will be presented.
Outcome/Objectives:
1. Understand the rationale for integrating PTSD treatment into DBT.
2. Outline the basic structure and procedures of the DBT Prolonged Exposure protocol for PTSD.
3. Review research findings evaluating the safety and effectiveness of the treatment.
February 19, 2020: Dissociation, Somatization, and Other Challenging Presentations of PTSD
Abigail Angkaw, PhD
Challenging presentations of PTSD, particularly dissociation and somatization trauma reactions, sometimes lead clinicians to hesitate offering evidence-based PTSD treatment. This course will help clinicians identify and understand dissociation and somatization presentations as trauma reactions within a PTSD case conceptualization framework, and will include reviewing clinical suggestions to support first-line evidence-based PTSD treatment for Veterans with these challenging presentations.
Outcome/Objectives:
1. Describe how individuals with PTSD may present with dissociation and somatization;
2. Discuss the rationale for not immediately excluding individuals with PTSD and dissociation or somatization reactions from evidence-based treatments for PTSD;
3. Identify methods to address dissociation and somatization PTSD reactions within evidence-based PTSD treatment.
February 5, 2020: Clinical and administrative applications of the PTSD-Repository Clinical Trials Database
Maya O’Neil, Ph.D., Jessica Hamblen, PhD, Tamara Cheney, MD
The development and use of evidence-based treatments for PTSD remains an important VA mission. This requires PTSD research that can inform and positively impact patient care. This presentation will highlight the relevance and effective use of the national PTSD repository for VA clinicians, educators, and researchers.
Outcome/Objectives:
1. Understand the rationale behind developing the PTSD-Repository;
2. Identify key patient, study, and outcome variables included in the PTSD-Repository;
3. Learn how to use the PTSD-Repository for clinical, administrative, educational, or research purposes.
January 15, 2020: Unconventional interventions for PTSD: State of the evidence
Paul Holtzheimer, MD, MSCR
Currently, several nonpharmacologic biological treatments are being investigated for the treatment of trauma. This presentation will explore the current evidence base for the use of these treatments, such as stellate ganglion block and hyperbaric oxygen, in PTSD treatment.
Outcome/Objectives:
1. describe various proposed non-pharmacologic biological treatements for PTSD
2. discuss the regulatory processes that provide safety oversight for these interventions; and
3. identify the safety and efficay data for focal brain stimulation in PTSD treatment.
December 18, 2019: Focal Brain Stimulation for PTSD
Paul Holtzheimer, MD, MSCR
Currently, several nonpharmacologic biological treatments are being investigated for the treatment of PTSD. This presentation will focus on the current evidence base for a particularly promising clinical treatment, focal brain stimulation, including potential benefits and risks.
Outcome/Objectives:
1. Describe the neural circuit paradigm that supports the use of focal brain stimulation for PTSD;
2. Summarize the rationale for using focal brain stimulation to treat PTSD; and
3. Identify the safety and efficay data for focal brain stimulation in PTSD treatment.
December 4, 2019: Lethal means safety: How clinicians can have the conversation
Bridget Matarazzo, PsyD
Lethal means safety is an important part of suicide prevention and risk assessment, one of the highest mental health priorities in VHA. This presentation will provide practical guidelines for clinicians for discussing lethal means safety with their patients in order to lower suicide risk.
Outcomes/Objectives:
1. Explain the importance of discussing lethal means safety with patients
2. Identify patients with whom providers should discuss lethal means safety
3. Discuss safe storage practices for firearms and medications
November, 2019: Quality of Care and Patient Outcomes Following Discontinuation of Long-Term Opioid Therapy in High-Risk Patients
Travis Lovejoy, PhD
The effective treatment of chronic pain is one of the greatest challenges for clinicians. Just as challenging is tapering and discontinuation of long-term opioids. This presentation will discuss these challenges that clinicians face with high-risk patients, and will offer perspectives on clinical outcomes and optimizing quality of care after opioid discontinuation.
Outcome/Objectives
1. Describe historical trends in opioid prescribing in the U.S.
2. Identify the consequences of opioid taper and discontinuation among long-term opioid users
3. Characterize changes in patients’ pain following discontinuation of long-term opioid therapy
November 6, 2019: Diagnosing ADHD in Adults, and Considering Treatment Options
Whitney Black, MD
One of the most challenging psychiatric illnesses to diagnose and treat is ADHD. Symptoms can overlap with several other conditions, and accurate diagnosis is dependent on an estimation of patient functioning going back to childhood and adolescence. Moreover, treatment options include the appropriate use of controlled substances with potential for misuse. This presentation will focus on these important clinical issues, and it will include considerations particularly relevant to the care of Veterans and healthcare teams.
Outcome/Objectives
1. Identify evidence-based screening measures when diagnosing ADHD
2. Describe strategies for psychostimulant titration trials in adult patients; and
3. Describe the role for non-stimulant medications in treatment of adults with ADHD.
October 16, 2019: The role of psychedelics in modern psychiatry: A review of the evidence base
Melissa Buboltz, MD, Aryan Sarparast, MD, Payton Sterba, MD, Jovo Vijanderan, MD
Sign up for email updates or access your subscriber preferences: https://public.govdelivery.com/accounts/USVHAVISN20/subscriber/new.
Use of these Materials and Finding VA Health Care
Please note that the health care information provided in these materials is for educational purposes only. It does not replace the role of a medical practitioner for advice on care and treatment. If you are looking for professional medical care, find your local VA healthcare center by using the VA Facilities Locator & Directory. This page may contain links that will take you outside of the Department of Veterans Affairs website. VA does not endorse and is not responsible for the content of the linked websites.
VA Web Disclaimers
Disclaimer of Endorsement: Reference herein to any specific commercial products, process, or service by trade name, trademark, manufacturer, or otherwise, does not necessarily constitute or imply its endorsement, recommendation, or favoring by the United States Government. The views and opinions of authors expressed herein do not necessarily state or reflect those of the United States Government, and shall not be used for advertising or product endorsement purposes.
Disclaimer of Hyperlinks: The appearance of external hyperlinks does not constitute endorsement by the Department of Veterans Affairs of the linked websites, or the information, products or services contained therein. For other than authorized VA activities, the Department does not exercise any editorial control over the information you may find at these locations. All links are provided with the intent of meeting the mission of the Department and the VA website. Please let us know about existing external links which you believe are inappropriate and about specific additional external links which you believe ought to be included.
Disclaimer of Liability: With respect to documents available from this server, neither the United States Government nor any of its employees, makes any warranty, express or implied, including the warranties of merchantability and fitness for a particular purpose, or assumes any legal liability or responsibility for the accuracy, completeness, or usefulness of any information, apparatus, product, or process disclosed, or represents that its use would not infringe privately owned rights.
Reference from this web page or from any of the information services sponsored by the VA to any non-governmental entity, product, service or information does not constitute an endorsement or recommendation by the VA or any of its employees. We are not responsible for the content of any "off-site" web pages referenced from this server.
Disclaimer: The sharing of any non-VA information does not constitute an endorsement of products or services on the part of the VA.
![]()
VA Regional Offices
 The Veterans Benefits Administration (VBA) helps service members transition out of military service, and assists with Veterans with education, home loans, life insurance and much more. Service members, Veterans, their families, and Survivors are invited to request information on VA Benefits including disability compensation, pension, fiduciary, education, Veteran Readiness and Employment (VR&E), Home Loans, and Insurance. In addition to information on VA Benefits Veterans may initiate an intent to file and request assistance with filing compensation and pension claims. Visit regional office websites to learn about the services the regional office provides, directions to the facility, hours of operation, and the leadership team that serves the regional office.
The Veterans Benefits Administration (VBA) helps service members transition out of military service, and assists with Veterans with education, home loans, life insurance and much more. Service members, Veterans, their families, and Survivors are invited to request information on VA Benefits including disability compensation, pension, fiduciary, education, Veteran Readiness and Employment (VR&E), Home Loans, and Insurance. In addition to information on VA Benefits Veterans may initiate an intent to file and request assistance with filing compensation and pension claims. Visit regional office websites to learn about the services the regional office provides, directions to the facility, hours of operation, and the leadership team that serves the regional office.
Find out if you can get VA health care as a Veteran
The following four categories of Veterans are not required to enroll but are urged to do so to permit better planning of health resources:
- Veterans with a service-connected (SC) disability rated at 50% or more.
- Veterans seeking care for a disability the military determined was incurred or aggravated in the line of duty, but which VA has not yet rated, within 12 months of discharge.
- Veterans seeking care for a SC disability only or under a special treatment authority.
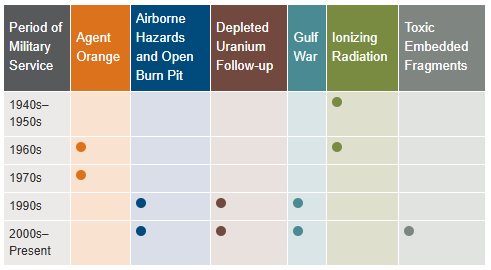
- Veterans seeking health registry examinations. VA’s health registry evaluation is a free, voluntary medical assessment for Veterans who may have been exposed to certain environmental hazards during military service. The evaluations alert Veterans to possible long-term health problems that may be related to exposure to specific environmental hazards during their military service. VA has established several health registries to track and monitor the health of specific groups of Veterans. You may be eligible to participate in one or more of these health registries: Agent Orange Registry, Airborne Hazards and Open Burn Pit Registry, Gulf War Registry (includes Operations Iraqi Freedom and New Dawn), Ionizing Radiation Registry, Depleted Uranium Follow-Up Program, and Toxic Embedded Fragment Surveillance Center. Use the chart below to help determine your eligibility.
Find out how to apply for VA health care benefits as a Veteran or service member. For other mental health services, contact a VA medical center for information on eligibility and treatment options.
Community Care (Mission Act)
The MISSION Act became law in 2018, bringing the VA’s previous Veterans Choice Program to an end and establishing the Community Care Program. VA provides health care for Veterans from providers in your local community outside of VA. Veterans may be eligible to receive care from a community provider when VA cannot provide the care needed. This care is provided on behalf of and paid for by VA. Community care is also available to Veterans based on certain conditions and eligibility requirements, and in consideration of a Veteran’s specific needs and circumstances. VA offers urgent care services to eligible Veterans at in-network urgent care clinics to treat minor injuries and illnesses that are not life-threatening, such as colds, strep throat, sprained muscles, and skin and ear infections. Community care must be first authorized by VA before a Veteran can receive care from a community provider.
Vet Centers in VISN 20
 Vet Centers in VISN 20 are community-based counseling centers that provide a wide range of social and psychological services, including professional readjustment counseling to eligible Veterans, active-duty Army, Navy, Marine Corp, Air Force, Space Force, and Coast Guard service members, including National Guard and Reserve components, and their families. 1-877-927-8387 is an around the clock confidential call center where combat Veterans and their families can call to talk about their military experience or any other issue they are facing in their readjustment to civilian life. The staff is comprised of combat Veterans from several eras as well as families members of combat Veterans. This benefit is prepaid through the Veteran’s military service.
Vet Centers in VISN 20 are community-based counseling centers that provide a wide range of social and psychological services, including professional readjustment counseling to eligible Veterans, active-duty Army, Navy, Marine Corp, Air Force, Space Force, and Coast Guard service members, including National Guard and Reserve components, and their families. 1-877-927-8387 is an around the clock confidential call center where combat Veterans and their families can call to talk about their military experience or any other issue they are facing in their readjustment to civilian life. The staff is comprised of combat Veterans from several eras as well as families members of combat Veterans. This benefit is prepaid through the Veteran’s military service.
Alaska
| Anchorage Vet Center (Anchorage, AK) | Fairbanks Vet Center (Fairbanks, AK) |
| Kenai Vet Center Outstation (Soldotna, AK) | Wasilla Vet Center (Wasilla, AK) |
Idaho
| Boise Vet Center (Boise, ID) | East Idaho Vet Center (Idaho Falls, ID) |
Oregon
| Central Oregon Vet Center (Bend, OR) | Eugene Vet Center (Eugene, OR) |
| Grants Pass Vet Center (Grants Pass, OR) | Portland, OR Vet Center (Portland, OR) |
| Salem Vet Center (Salem, OR) |
Washington
Plan your trip to VA
 In 1946, Veterans Canteen Service (VCS) was established by law to provide comfort and well-being to America’s Veterans. With our many retail stores, cafés and coffee shops across the country, we serve those who have served our country. We are a self-sustaining entity providing merchandise and services to Veterans enrolled in VA’s healthcare system, their families, caregivers, VA employees, volunteers and visitors. We are honored to give back to the VA community through many programs established for the health and well-being of our nation’s heroes. Revenues generated from VCS are used to support a variety of programs, such as VA’s Rehabilitation Games, Fisher Houses, Poly-Trauma Centers for OIF/OEF/OND Veterans, disaster relief efforts, Substance Abuse Cessation, VA’s Homelessness initiatives, Women Veterans, Veteran Suicide Prevention and other activities.
In 1946, Veterans Canteen Service (VCS) was established by law to provide comfort and well-being to America’s Veterans. With our many retail stores, cafés and coffee shops across the country, we serve those who have served our country. We are a self-sustaining entity providing merchandise and services to Veterans enrolled in VA’s healthcare system, their families, caregivers, VA employees, volunteers and visitors. We are honored to give back to the VA community through many programs established for the health and well-being of our nation’s heroes. Revenues generated from VCS are used to support a variety of programs, such as VA’s Rehabilitation Games, Fisher Houses, Poly-Trauma Centers for OIF/OEF/OND Veterans, disaster relief efforts, Substance Abuse Cessation, VA’s Homelessness initiatives, Women Veterans, Veteran Suicide Prevention and other activities.
VCS operates over 200 Patriot Stores in Veterans Administration (VA) Medical Centers nationwide. Many of our stores have been recently updated and expanded to provide our customers with a modern, clean and comfortable shopping experience. Our stores welcome our customers with wider aisles, wood-like floors, enhanced lighting and directional signage. PatriotStores have expanded hours of operation to provide service for customers on weekends at most locations.
The Patriot Cafe is the best place in the VA Medical Center to enjoy delicious, freshly prepared breakfast or lunch served hot or cold each weekday. Providing Veterans, their families, VA employees, volunteers and visitors a place to relax and enjoy a meal or take-out for their convenience. With a wide variety of food from traditional comfort food, specialized menu selections and a large assortment of healthy choices; there is something for everyone's taste buds.
Hospital Service Directory
To find out whether there is a van near you use the Disabled American Veterans (DAV) Hospital Service Coordinator Directory to contact your nearest HSC for information or assistance. Please remember that the DAV Transportation Network is staffed by volunteers; therefore, it is unable to cover every community. The vans are driven by volunteers, and the rides coordinated by more than 133 Hospital Service Coordinators around the country. Our nation’s heroes travel around the globe to protect our freedoms—it’s only right that we return their dedication. Volunteering to drive a Vet ensures that even those living remotely from VA hospitals can make their appointments and never go without the treatment they need. Learn more about the DAV transportation network through the VISN 20 NewsFlash Resources section.
 Today's VHA - the largest of the three administrations that comprise the VA - continues to meet Veterans' changing medical, surgical, and quality-of-life needs. VHA is the largest integrated health care system in the United States, providing care at 1,321 health care facilities, including 172 VA Medical Centers and 1,138 outpatient sites of care of varying complexity (VHA outpatient clinics) to over 9 million Veterans enrolled in the VA health care program. There are 18 Veterans Integrated Service Networks (VISNs) in VHA operating as regional systems of care to better meet local health care needs and provides greater access to care. In the Pacific Northwest, VISN 20 serves Veterans in Alaska, Oregon, Washington, most of Idaho, and one county each in California and Montana. Spanning 23% of the US land mass, VISN 20 is the largest geographic region of VA. Operating across three time zones over 817,417 square miles, VISN 20 is home to 273 federally recognized American Indian and Alaskan Native tribes. According to DoD, American Indians and Alaska Natives have one of the highest representations in the United States Armed Forces. VA consults with American Indian and Alaska Native tribal governments to develop partnerships that enhance access to services and benefits by Veterans and their families. VA is committed to ensuring that Native American Veterans and their families are able to utilize all benefits and services they are entitled to receive. As of the end of FY2024, 39% of VISN 20 enrollees resided in rural or highly rural areas.
Today's VHA - the largest of the three administrations that comprise the VA - continues to meet Veterans' changing medical, surgical, and quality-of-life needs. VHA is the largest integrated health care system in the United States, providing care at 1,321 health care facilities, including 172 VA Medical Centers and 1,138 outpatient sites of care of varying complexity (VHA outpatient clinics) to over 9 million Veterans enrolled in the VA health care program. There are 18 Veterans Integrated Service Networks (VISNs) in VHA operating as regional systems of care to better meet local health care needs and provides greater access to care. In the Pacific Northwest, VISN 20 serves Veterans in Alaska, Oregon, Washington, most of Idaho, and one county each in California and Montana. Spanning 23% of the US land mass, VISN 20 is the largest geographic region of VA. Operating across three time zones over 817,417 square miles, VISN 20 is home to 273 federally recognized American Indian and Alaskan Native tribes. According to DoD, American Indians and Alaska Natives have one of the highest representations in the United States Armed Forces. VA consults with American Indian and Alaska Native tribal governments to develop partnerships that enhance access to services and benefits by Veterans and their families. VA is committed to ensuring that Native American Veterans and their families are able to utilize all benefits and services they are entitled to receive. As of the end of FY2024, 39% of VISN 20 enrollees resided in rural or highly rural areas.
VA Puget Sound Health Care System (VAPSHCS) serves Veterans from a five-state area in the Pacific Northwest with two main divisions: American Lake VA Medical Center and Seattle VA Medical Center. Veterans Medical Centers are also located in Spokane, Vancouver, and Walla Walla. VA Outpatient Clinics and Vet Centers are located in Bellingham, Bellevue, Bremerton, Edmunds, Everett, Federal Way, Lacey, Mount Vernon, Olympia, Port Angeles, Puyallup, Richland, Renton, Silverdale, Seattle, Spokane, Union Gap, Vancouver, Walla Walla, Wenatchee, and Yakima.
VA Portland Health Care System (VAPORHCS) serves Veterans in Oregon and Southwest Washington with two main divisions: Portland VA Medical Center and Vancouver VA Medical Center. Veterans Medical Centers are also located in Roseburg, White City, and Vancouver, Washington. VA Outpatient Clinics and Vet Centers are located in Astoria, Bend, Boardman, Brookings, Eugene, Fairview, Grants Pass, Hines, Hillsboro, Klamath Falls, LaGrande, Lincoln City, Newport, Portland, Salem, The Dalles, and West Linn.