MIRECC / CoE
2020 VISN 20 MIRECC Staff Research Articles and Presentations
VISN 20 MIRECC Staff Research Articles and Presentations
The findings of NW MIRECC research are disseminated through MIRECC Presents, lectures and presentations, and publications. Below is a list of publications and presentations by VISN 20 NW MIRECC researchers and fellowship program faculty that were published in 2020.
Bahraini, N. H., Matarazzo, B. E., Barry, C., Post, E., Forster, J., Dollar, K., Dobscha, S., & Brenner, L. (2020). Protocol: examining the effectiveness of an adaptive implementation intervention to improve uptake of the VA suicide risk identification strategy: a sequential multiple assignment randomized trial. Implementation Science, 15 (1), 58. doi:10.1186/s13012-020-01019-6
Bourassa, K. J., Edwards-Steward, A., Smolenski, D. J., Campbell, S. B., Reger, G. M., & Norr, A. M. (2020). The impact of prolonged exposure therapy on social support and PTSD symptoms. Journal of Affective Disorders, 260, 410-417. doi:10.1016/j.jad.2019.09.036
Bourassa, K. J., Stevens, E., Katz, A. C., Rothbaum, B. O., Reger, G. M., & Norr, A. M. (2020). The impact of exposure therapy on stigma and mental health treatment attitudes among active duty U.S. soldiers with combat related PTSD. Journal of Psychiatric Research, 126, 98-104. doi:10.1016/j.jpsychires.2020.05.005
Bourassa, K., Stevens, E., Katz, A., Rothbaum, B., Reger, G., & Norr, A. M. (2020). The Impact of Exposure Therapy on Resting Heart Rate and Heart Rate Reactivity Among Active-Duty Soldiers With Posttraumatic Stress Disorder. Psychosomatic Medicine, 82 (1), 108-114. doi:10.1097/PSY.0000000000000758
Braun, M., & Iliff, J. J. (2020). Chapter Fifteen: The impact of neurovascular, blood-brain barrier, and glymphatic dysfunction in neurodegenerative and metabolic diseases. International Review of Neurobiology, 154, 413-436.
Chen, D., Latimer, C., Yagi, M., Ndugga-Kabuye, M., Heigham, E., Jayadev, S., Meabon, J., Gomez, C., Keene, C., Cook, D. G., Raskind, W., & Bird, T. (2020). Heterozygous STUB1missense variants cause ataxia, cognitive decline, and STUB1 mislocalization. Neurology Genetics, 6 (2), e397. doi:10.1212/NXG.0000000000000397
Coffey, K. R., Lesiak, A. J., Cohen, J., Liang, K., Chavkin, C., & Neumaier, J. F. (2020). Sequencing the serotonergic neuron translatome reveals a new role for FkbpS in stress. Molecular Psychiatry. Advance online publication. doi:10.1038/s41380-020-0750-4
Coffey, K. R., Marx, R. G., Vo, E. K., Nair., S. G., & Neumaier, J. F. (2020). Chemogenetic inhibition of lateral habenula projections to the dorsal raphe nucleus reduces passive coping and perseverative reward seeking in rats. Neuropsychopharmacology, 45, 1115–1124.
Cross, D., Meabon, J., Cline, M., Richards, T., Stump, A., Cross, C., Minoshima, S., Banks, W., & Cook, D. G. (2019). Paclitaxel Reduces Brain Injury from Repeated Head Trauma in Mice. Journal of Alzheimer's Disease, 67 (3), 859-874. doi:10.3233/jad-180871
Dennis, E. L., Disner, S. G., Fani, N., Salminen, L. E., Logue, M. W., Clarke, E., Haswell, C., Averill, C. L., Baugh, L. A., Bomyea, J., Hayes, J. P., Krystal, J. H., Li, G., May, G. J., Menefee, D. S., Nelson, S. M., Simmons, A. N., Sullivan, D. R., Abdallah, C., Gordon, E. M., Kremen, W. S., Stein, M., Tate, D. F., Wee, N. J., der, V., Wang, L., Wilde, E. A., Thompson, P. M., Kochunov, P., Jahanshad, N., & Morey, R. (2019). Altered white matter microstructural organization in post-traumatic stress disorder across 3,049 adults: Results from the PGC-ENIGMA PTSD consortium. Molecular Psychiatry. Advance online publication. doi:10.1038/s41380-019-0631-x
Figlewicz, D. P., & Witkamp, R. (2020). Fatty acids as cell signals in ingestive behaviors. Physiology and Behavior, 223, 112985. doi:10.1016/j.physbeh.2020.112985
Freeman, M., Ayers, C., Kondo, K., Noonan, K., O’Neil, M., Morasco, B., & Kansagara, D. (2019). Guided imagery, biofeedback, and hypnosis: a map of the evidence. Evidence-based Synthesis Program (ESP) Portland VA Health Care System Project #05-225.
Ghai, V., Fallen, S., Baxter, D., Scherler, K., Kim, T., Zhou, Y., Meabon, J., Logsdon, A., Banks, W., Schindler, A., Cook, D. G., Peskind, E. R., Lee, I., & Wang, K. (2020). Alterations in Plasma microRNA and Protein Levels in War Veterans with Chronic Mild Traumatic Brain Injury. Journal of Neurotrauma, 37 (12), 1418-1430. doi:10.1089/neu.2019.6826
Hendrickson, R. C., Nishanth, J. H., & Michael, S. (2020). Diagnostic prevalence of common psychiatric comorbidities of alcohol use disorders in India: a systematic review and discussion of the implications. International Journal of Mental Health and Addiction, 17(5):, 1268-1296.
Hendrickson, R. C., Thomas, R. G., Schork, N. J., & Raskind, M. A. (2020). Optimizing aggregated N-of-1 trial designs for predictive biomarker validation: statistical methods and theoretical findings. Frontiers in Digital Health. doi:10.3389/fdgth.2020.00013
Jarrahi, A., Braun, M., Ahluwalia, M., Gupta, R., Wilson, M., Munie, S., Ahluwalia, P., Vender, J., Vale, F., Dhandapani, K., & Vaibhav, K. (2020). Revisiting Traumatic Brain Injury: From Molecular Mechanisms to Therapeutic Interventions. Biomedicines, 8 (10), 389. doi:10.3390/biomedicines8100389
Katz, A., Norr, A. M., Buck, B., Fantelli, E., Edwards-Stewart, A., Koenen-Woods, P., Zetocha, K., Smolenski, D., Holloway, K., Rothbaum, B., Difede, J., Rizzo, A., Skopp, N., Mishkind, M., Gahm, G., Reger, G., & Andrasik, F. (2020). Changes in physiological reactivity in response to the trauma memory during prolonged exposure and virtual reality exposure therapy for posttraumatic stress disorder. Psychological Trauma: Theory, Research, Practice, and Policy, 12 (7), 756-764. doi:10.1037/tra0000567
Kondo, K. K., Noonan, K. M., Freeman, M., Ayers, C. K., Morasco, B., & Kansagara, D. (2019). Efficacy of biofeedback for medical conditions: an evidence map. Journal of General Internal Medicine, 34, 2883-2893.
Kondo, K., Morasco, B., Nugent, S., Ayers, C., O’Neil, M., Freeman, M., Paynter, R., & Kansagara, D. (2019). Pharmacotherapy for the treatment of cannabis use disorder: a systematic review. Evidence-based Synthesis Program (ESP) Portland VA Health Care System Project #05-225.
Lewis, M., & Loverich, T. M. (2019). Measuring experiential avoidance and posttraumatic stress in families. Behavioral Sciences, 9, 1-16.
Logsdon, A., Schindler, A., Meabon, J., Yagi, M., Herbert, M., Banks, W., Raskind, M. A., Marshall, D., Keene, C., Perl, D., Peskind, E. R., & Cook, D. G. (2020). Nitric oxide synthase mediates cerebellar dysfunction in mice exposed to repetitive blast-induced mild traumatic brain injury. Scientific Reports, 10 (1), 9420. doi:10.1038/s41598-020-66113-7
Mahmood, Z., Clark, J., Jak, A. J., Huckans, M., O'Neil, M., Roost, M., Williams, R., Pagulayan, K. F., Turner, A., Storzbach, D., & Twamley, E. W. (2020). Predictors of Intervention Adherence in Compensatory Cognitive Training for Veterans With a History of Mild Traumatic Brain Injury. Journal of Head Trauma Rehabilitation, 36(1), 20-24. doi:10.1097/htr.0000000000000596
Maloy, P. E., Iacocca, M. O., & Morasco, B. (2019). Implementing guidelines for treating chronic pain with prescription opioids. American Journal of Nursing, 119, 22-29.
Mastarone, G. L., Wyse, J., Wilbur, E., Morasco, B., Saha, S., & Carlson, K. F. (2020). Barriers to utilization of prescription drug monitoring programs among prescribing physicians and advanced practice registered nurses at Veterans Health Administration facilities in Oregon. Pain Medicine, 21, 695-703.
Morasco, B., Adams, M. H., Maloy, P. E., Hooker, E. R., Iacocca, M. O., Krebs, E. E., Carr, T. P., Lovejoy, T. I., Saha, S., & Dobscha, S. (2020). Research methods and baseline findings of the Improving the Safety of Opioid Therapy (ISOT) cluster randomized trial. Contemporary Clinical Trials, 90, 105957.
Morasco, B., Smith, N., Dobscha, S., Deyo, R. A., Hyde, S., & Yarborough, B...J...H... (2020). Outcomes of prescription opioid dose escalation for chronic pain: Results from a prospective cohort study. Pain, 16, 1332-1340.
Nair, S. G., Smirnov, D., Estabrook, M., Chisholm, A. D., Silva, P., & Neumaier, J. F. (2020). Effect of chemogenetic inhibition of lateral habenula neuronal activity on cocaine- and food-seeking behaviors in the rat. Addiction Biollogy. Advance online publication.
Norr, A. M., Katz, A., Nguyen, J., Lehavot, K., Schmidt, N., & Reger, G. (2020). Pilot trial of a transdiagnostic computerized anxiety sensitivity intervention among VA primary care patients. Psychiatry Research, 293, 113394. doi:10.1016/j.psychres.2020.113394
O’Neil, M., Harik, J. M., McDonagh, M. S., Cheney, T. P., Hsu, F. C., Cameron, D. C., Carlson, K. F., Norman, S. B., & Hamblen, J. L. (2020). Development of the PTSD-Repository: A publicly available repository of randomized controlled trials for posttraumatic stress disorder. Journal of Traumatic Stress, 33, 410-419. doi:10.1002/jts.22520
Pagulayan, K. F., Petrie, E. C., MD, Cook, D. G., Hendrickson, R. C., Rau, H., Reilly, M., Mayer, C., Meabon, J., Raskind, M. A., Peskind, E. R., & Kleinhans, N. (2020). Effect of blast-related mTBI on the working memory system: a resting state fMRI study. Brain Imaging and Behavior, 14 (4), 949-960. doi:10.1007/s11682-018-9987-9
Raskind, M. A. (2020). Toward a personalized medicine approach to trauma-related nightmares. Sleep Medicine Reviews, 50, 101272. doi:10.1016/j.smrv.2020.101272
Ray, L., Iliff, J. J., & Heys, J. (2019). Analysis of convective and diffusive transport in the brain interstitium. Fluids and Barriers of the CNS. doi:10.1186/s12987-019-0126-9
Reddy, V., Grogan, D., Ahluwalia, M., Salles, É. L., Ahluwalia, P., Khodadadi, H., Alverson, K., Nguyen, A., Raju, S. P., Gaur, P., Braun, M., Vale, F. L., Costigliola, V., Dhandapani, K., Baban, B., & Vaibhav, K. (2020). Targeting the endocannabinoid system: a predictive, preventive, and personalized medicine-directed approach to the management of brain pathologies. EPMA Journal, 11, 217–250.
Shibata-Germanos, S., Goodman, J., Grieg, A., Trivedi, C., Benson, B., Foti, S., Faro, A., Castellan, R., Correra, R., Barber, M., Ruhrberg, C., Weller, R., Lashley, T., Iliff, J. J., Hawkins, T., & Rihel, J. (2020). Structural and functional conservation of non-lumenized lymphatic endothelial cells in the mammalian leptomeninges. Acta Neuropathologica, 139 (2), 383-401. doi:10.1007/s00401-019-02091-z
Shulman, G. P., Buck, B. E., Gahm, G. A., Reger, G. M., & Norr, A. M. (2019). Effectiveness of the Intent to Complete and Intent to Attend Intervention to Predict and Prevent Posttraumatic Stress Disorder Treatment Drop Out Among Soldiers. Journal of Traumatic Stress, 32 (5), 784-790. doi:10.1002/jts.22427
Sorg, S., Merritt, V., Clark, A., Werhane, M., Holiday, K., Schiehser, D. M., Bondi, M., & Delano-Wood, L. (2020). Elevated Intraindividual Variability in Executive Functions and Associations with White Matter Microstructure in Veterans with Mild Traumatic Brain Injury. Journal of the International Neuropsychological Society, 2, 1-10. doi:10.1017/S1355617720000879
Stewart, T., Bai, L., Li, X., Xu, T., Iliff, J. J., Shi, M., Zheng, D., Yuan, L., Wei, T., Yang, X., & Zhang, J. (2020). Coniferaldehyde attenuates Alzheimer’s pathology via activation of Nrf2 and its targets. Theranostics, 10(1), 179-200.
Sweigert, J., Pagulayan, K. F., Greco, G., Blake, M., Larimer, M., & Kleinhans, N. (2020). A multi-modal investigation of cerebellar integrity associated with high risk cannabis use. Addiction Biology, 25(6), e12839. doi:10.1111/adb.12839
Vaibhav, K. *., Braun, M., Alverson, K., Khodadadi, H., Kutiyanawalla, A., Ward, A., Banerjee, C., Sparks, T., Malik, A., Rashid, M. H., Khan, M. B., Waters, M. F., Hess, D. C., Arbab, A. S., Vender, J. R., Hoda, N., Baban, B., & Dhandapani, K. M. (2020). Neutrophil extracellular traps exacerbate neurological deficits after traumatic brain injury. Science Advances, 6(22), eaax8847.
Verstaen, A., Rau, H., & Trittschuh, E. H. (2020). Healthy Aging Project-Brain: a Psychoeducational and Motivational Group for Older Veterans. Federal Practitioner : for the Health Care Professionals of the VA, DoD, and PHS, 37(7), 309–315.
Wheeler, J., McMillan, P., Strovas, T., Liachko, N. F., Amlie-Wolf, A., Kow, R., Klein, R., Szot, P., Robinson, L., Guthrie, C., Saxton, A., Kanaan, N., Raskind, M. A., Peskind, E. R., Trojanowski, J., Lee, V., Wang, L., Keene, C., Bird, T., Schellenberg, G., & Kraemer, B. C. (2019). Activity of the poly(A) binding protein MSUT2 determines susceptibility to pathological tau in the mammalian brain. Science Translational Medicine, 11 (523), eaao6545. doi:10.1126/scitranslmed.aao6545
Yarborough, B...J...H..., Stumbo, S. P., Stoneburner, A., Smith, N. X., Dobscha, S., Deyo, R. A., & Morasco, B. (2019). Correlates of benzodiazepine use and adverse outcomes among patients prescribed long-term opioid therapy. Pain Medicine, 20, 1148-1155.
Sign up for email updates or access your subscriber preferences: https://public.govdelivery.com/accounts/USVHAVISN20/subscriber/new.
Use of these Materials and Finding VA Health Care
Please note that the health care information provided in these materials is for educational purposes only. It does not replace the role of a medical practitioner for advice on care and treatment. If you are looking for professional medical care, find your local VA healthcare center by using the VA Facilities Locator & Directory. This page may contain links that will take you outside of the Department of Veterans Affairs website. VA does not endorse and is not responsible for the content of the linked websites.
VA Web Disclaimers
Disclaimer of Endorsement: Reference herein to any specific commercial products, process, or service by trade name, trademark, manufacturer, or otherwise, does not necessarily constitute or imply its endorsement, recommendation, or favoring by the United States Government. The views and opinions of authors expressed herein do not necessarily state or reflect those of the United States Government, and shall not be used for advertising or product endorsement purposes.
Disclaimer of Hyperlinks: The appearance of external hyperlinks does not constitute endorsement by the Department of Veterans Affairs of the linked websites, or the information, products or services contained therein. For other than authorized VA activities, the Department does not exercise any editorial control over the information you may find at these locations. All links are provided with the intent of meeting the mission of the Department and the VA website. Please let us know about existing external links which you believe are inappropriate and about specific additional external links which you believe ought to be included.
Disclaimer of Liability: With respect to documents available from this server, neither the United States Government nor any of its employees, makes any warranty, express or implied, including the warranties of merchantability and fitness for a particular purpose, or assumes any legal liability or responsibility for the accuracy, completeness, or usefulness of any information, apparatus, product, or process disclosed, or represents that its use would not infringe privately owned rights.
Reference from this web page or from any of the information services sponsored by the VA to any non-governmental entity, product, service or information does not constitute an endorsement or recommendation by the VA or any of its employees. We are not responsible for the content of any "off-site" web pages referenced from this server.
Disclaimer: The sharing of any non-VA information does not constitute an endorsement of products or services on the part of the VA.
![]()
VA Regional Offices
 The Veterans Benefits Administration (VBA) helps service members transition out of military service, and assists with Veterans with education, home loans, life insurance and much more. Service members, Veterans, their families, and Survivors are invited to request information on VA Benefits including disability compensation, pension, fiduciary, education, Veteran Readiness and Employment (VR&E), Home Loans, and Insurance. In addition to information on VA Benefits Veterans may initiate an intent to file and request assistance with filing compensation and pension claims. Visit regional office websites to learn about the services the regional office provides, directions to the facility, hours of operation, and the leadership team that serves the regional office.
The Veterans Benefits Administration (VBA) helps service members transition out of military service, and assists with Veterans with education, home loans, life insurance and much more. Service members, Veterans, their families, and Survivors are invited to request information on VA Benefits including disability compensation, pension, fiduciary, education, Veteran Readiness and Employment (VR&E), Home Loans, and Insurance. In addition to information on VA Benefits Veterans may initiate an intent to file and request assistance with filing compensation and pension claims. Visit regional office websites to learn about the services the regional office provides, directions to the facility, hours of operation, and the leadership team that serves the regional office.
Find out if you can get VA health care as a Veteran
The following four categories of Veterans are not required to enroll but are urged to do so to permit better planning of health resources:
- Veterans with a service-connected (SC) disability rated at 50% or more.
- Veterans seeking care for a disability the military determined was incurred or aggravated in the line of duty, but which VA has not yet rated, within 12 months of discharge.
- Veterans seeking care for a SC disability only or under a special treatment authority.
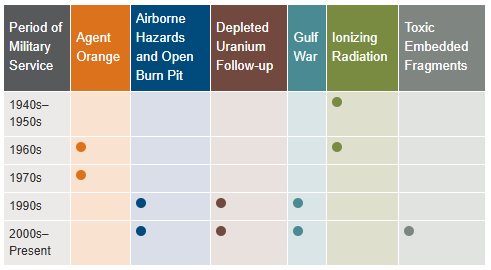
- Veterans seeking health registry examinations. VA’s health registry evaluation is a free, voluntary medical assessment for Veterans who may have been exposed to certain environmental hazards during military service. The evaluations alert Veterans to possible long-term health problems that may be related to exposure to specific environmental hazards during their military service. VA has established several health registries to track and monitor the health of specific groups of Veterans. You may be eligible to participate in one or more of these health registries: Agent Orange Registry, Airborne Hazards and Open Burn Pit Registry, Gulf War Registry (includes Operations Iraqi Freedom and New Dawn), Ionizing Radiation Registry, Depleted Uranium Follow-Up Program, and Toxic Embedded Fragment Surveillance Center. Use the chart below to help determine your eligibility.
Find out how to apply for VA health care benefits as a Veteran or service member. For other mental health services, contact a VA medical center for information on eligibility and treatment options.
Community Care (Mission Act)
The MISSION Act became law in 2018, bringing the VA’s previous Veterans Choice Program to an end and establishing the Community Care Program. VA provides health care for Veterans from providers in your local community outside of VA. Veterans may be eligible to receive care from a community provider when VA cannot provide the care needed. This care is provided on behalf of and paid for by VA. Community care is also available to Veterans based on certain conditions and eligibility requirements, and in consideration of a Veteran’s specific needs and circumstances. VA offers urgent care services to eligible Veterans at in-network urgent care clinics to treat minor injuries and illnesses that are not life-threatening, such as colds, strep throat, sprained muscles, and skin and ear infections. Community care must be first authorized by VA before a Veteran can receive care from a community provider.
Vet Centers in VISN 20
 Vet Centers in VISN 20 are community-based counseling centers that provide a wide range of social and psychological services, including professional readjustment counseling to eligible Veterans, active-duty Army, Navy, Marine Corp, Air Force, Space Force, and Coast Guard service members, including National Guard and Reserve components, and their families. 1-877-927-8387 is an around the clock confidential call center where combat Veterans and their families can call to talk about their military experience or any other issue they are facing in their readjustment to civilian life. The staff is comprised of combat Veterans from several eras as well as families members of combat Veterans. This benefit is prepaid through the Veteran’s military service.
Vet Centers in VISN 20 are community-based counseling centers that provide a wide range of social and psychological services, including professional readjustment counseling to eligible Veterans, active-duty Army, Navy, Marine Corp, Air Force, Space Force, and Coast Guard service members, including National Guard and Reserve components, and their families. 1-877-927-8387 is an around the clock confidential call center where combat Veterans and their families can call to talk about their military experience or any other issue they are facing in their readjustment to civilian life. The staff is comprised of combat Veterans from several eras as well as families members of combat Veterans. This benefit is prepaid through the Veteran’s military service.
Alaska
| Anchorage Vet Center (Anchorage, AK) | Fairbanks Vet Center (Fairbanks, AK) |
| Kenai Vet Center Outstation (Soldotna, AK) | Wasilla Vet Center (Wasilla, AK) |
Idaho
| Boise Vet Center (Boise, ID) | East Idaho Vet Center (Idaho Falls, ID) |
Oregon
| Central Oregon Vet Center (Bend, OR) | Eugene Vet Center (Eugene, OR) |
| Grants Pass Vet Center (Grants Pass, OR) | Portland, OR Vet Center (Portland, OR) |
| Salem Vet Center (Salem, OR) |
Washington
Plan your trip to VA
 In 1946, Veterans Canteen Service (VCS) was established by law to provide comfort and well-being to America’s Veterans. With our many retail stores, cafés and coffee shops across the country, we serve those who have served our country. We are a self-sustaining entity providing merchandise and services to Veterans enrolled in VA’s healthcare system, their families, caregivers, VA employees, volunteers and visitors. We are honored to give back to the VA community through many programs established for the health and well-being of our nation’s heroes. Revenues generated from VCS are used to support a variety of programs, such as VA’s Rehabilitation Games, Fisher Houses, Poly-Trauma Centers for OIF/OEF/OND Veterans, disaster relief efforts, Substance Abuse Cessation, VA’s Homelessness initiatives, Women Veterans, Veteran Suicide Prevention and other activities.
In 1946, Veterans Canteen Service (VCS) was established by law to provide comfort and well-being to America’s Veterans. With our many retail stores, cafés and coffee shops across the country, we serve those who have served our country. We are a self-sustaining entity providing merchandise and services to Veterans enrolled in VA’s healthcare system, their families, caregivers, VA employees, volunteers and visitors. We are honored to give back to the VA community through many programs established for the health and well-being of our nation’s heroes. Revenues generated from VCS are used to support a variety of programs, such as VA’s Rehabilitation Games, Fisher Houses, Poly-Trauma Centers for OIF/OEF/OND Veterans, disaster relief efforts, Substance Abuse Cessation, VA’s Homelessness initiatives, Women Veterans, Veteran Suicide Prevention and other activities.
VCS operates over 200 Patriot Stores in Veterans Administration (VA) Medical Centers nationwide. Many of our stores have been recently updated and expanded to provide our customers with a modern, clean and comfortable shopping experience. Our stores welcome our customers with wider aisles, wood-like floors, enhanced lighting and directional signage. PatriotStores have expanded hours of operation to provide service for customers on weekends at most locations.
The Patriot Cafe is the best place in the VA Medical Center to enjoy delicious, freshly prepared breakfast or lunch served hot or cold each weekday. Providing Veterans, their families, VA employees, volunteers and visitors a place to relax and enjoy a meal or take-out for their convenience. With a wide variety of food from traditional comfort food, specialized menu selections and a large assortment of healthy choices; there is something for everyone's taste buds.
Hospital Service Directory
To find out whether there is a van near you use the Disabled American Veterans (DAV) Hospital Service Coordinator Directory to contact your nearest HSC for information or assistance. Please remember that the DAV Transportation Network is staffed by volunteers; therefore, it is unable to cover every community. The vans are driven by volunteers, and the rides coordinated by more than 133 Hospital Service Coordinators around the country. Our nation’s heroes travel around the globe to protect our freedoms—it’s only right that we return their dedication. Volunteering to drive a Vet ensures that even those living remotely from VA hospitals can make their appointments and never go without the treatment they need. Learn more about the DAV transportation network through the VISN 20 NewsFlash Resources section.
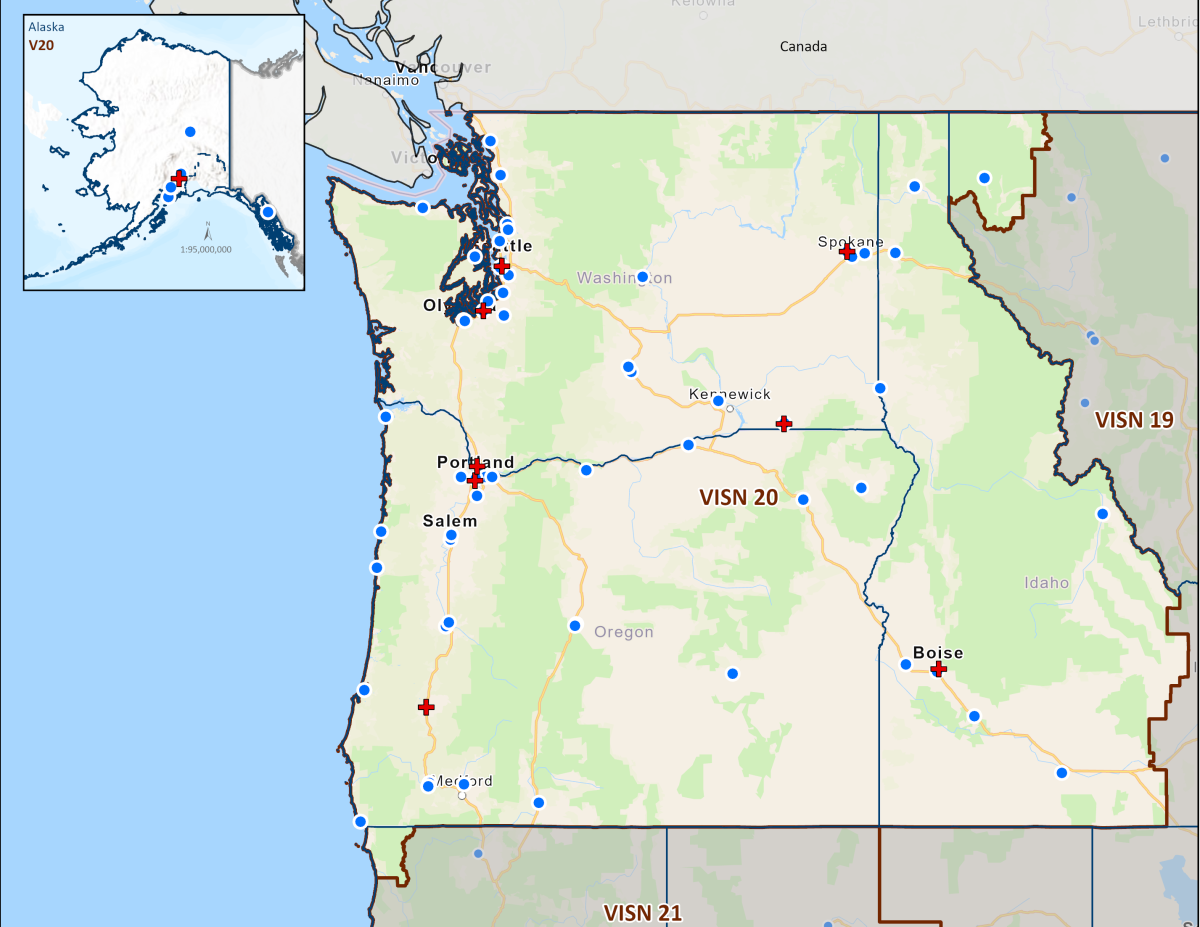 Today's VHA - the largest of the three administrations that comprise the VA - continues to meet Veterans' changing medical, surgical, and quality-of-life needs. VHA is the largest integrated health care system in the United States, providing care at 1,321 health care facilities, including 172 VA Medical Centers and 1,138 outpatient sites of care of varying complexity (VHA outpatient clinics) to over 9 million Veterans enrolled in the VA health care program. There are 18 Veterans Integrated Service Networks (VISNs) in VHA operating as regional systems of care to better meet local health care needs and provides greater access to care. In the Pacific Northwest, VISN 20 serves Veterans in Alaska, Oregon, Washington, most of Idaho, and one county each in California and Montana. Spanning 23% of the US land mass, VISN 20 is the largest geographic region of VA. Operating across three time zones over 817,417 square miles, VISN 20 is home to 273 federally recognized American Indian and Alaskan Native tribes. According to DoD, American Indians and Alaska Natives have one of the highest representations in the United States Armed Forces. VA consults with American Indian and Alaska Native tribal governments to develop partnerships that enhance access to services and benefits by Veterans and their families. VA is committed to ensuring that Native American Veterans and their families are able to utilize all benefits and services they are entitled to receive. As of the end of FY2024, 39% of VISN 20 enrollees resided in rural or highly rural areas.
Today's VHA - the largest of the three administrations that comprise the VA - continues to meet Veterans' changing medical, surgical, and quality-of-life needs. VHA is the largest integrated health care system in the United States, providing care at 1,321 health care facilities, including 172 VA Medical Centers and 1,138 outpatient sites of care of varying complexity (VHA outpatient clinics) to over 9 million Veterans enrolled in the VA health care program. There are 18 Veterans Integrated Service Networks (VISNs) in VHA operating as regional systems of care to better meet local health care needs and provides greater access to care. In the Pacific Northwest, VISN 20 serves Veterans in Alaska, Oregon, Washington, most of Idaho, and one county each in California and Montana. Spanning 23% of the US land mass, VISN 20 is the largest geographic region of VA. Operating across three time zones over 817,417 square miles, VISN 20 is home to 273 federally recognized American Indian and Alaskan Native tribes. According to DoD, American Indians and Alaska Natives have one of the highest representations in the United States Armed Forces. VA consults with American Indian and Alaska Native tribal governments to develop partnerships that enhance access to services and benefits by Veterans and their families. VA is committed to ensuring that Native American Veterans and their families are able to utilize all benefits and services they are entitled to receive. As of the end of FY2024, 39% of VISN 20 enrollees resided in rural or highly rural areas.
VA Medical Centers within VISN 20
Colonel Mary Louise Rasmuson Campus of the Alaska VA Healthcare System, Anchorage, Alaska
VA Boise Medical Center of the Boise VA Healthcare System, Boise, Idaho
VA Portland Medical Center of the Portland VA Healthcare System, Portland, Oregon
VA Roseburg Medical Center of the Roseburg VA Healthcare System, Roseburg, Oregon
VA White City Medical Center of the VA Southern Oregon Healthcare System, White City, Oregon
VA Seattle Medical Center of the VA Puget Sound Healthcare System, Seattle, Washington
Mann-Grandstaff Department of Veterans Affairs Medical Center, Spokane, Washington
Jonathan M. Wainwright Memorial VA Medical Center of the VA Walla Walla Healthcare System, Walla Walla, Washington
VA Puget Sound Health Care System (VAPSHCS) serves Veterans from a five-state area in the Pacific Northwest with two main divisions: American Lake VA Medical Center and Seattle VA Medical Center. Veterans Medical Centers are also located in Spokane, Vancouver, and Walla Walla. VA Outpatient Clinics and Vet Centers are located in Bellingham, Bellevue, Bremerton, Edmunds, Everett, Federal Way, Lacey, Mount Vernon, Olympia, Port Angeles, Puyallup, Richland, Renton, Silverdale, Seattle, Spokane, Union Gap, Vancouver, Walla Walla, Wenatchee, and Yakima.
VA Portland Health Care System (VAPORHCS) serves Veterans in Oregon and Southwest Washington with two main divisions: Portland VA Medical Center and Vancouver VA Medical Center. Veterans Medical Centers are also located in Roseburg, White City, and Vancouver, Washington. VA Outpatient Clinics and Vet Centers are located in Astoria, Bend, Boardman, Brookings, Eugene, Fairview, Grants Pass, Hines, Hillsboro, Klamath Falls, LaGrande, Lincoln City, Newport, Portland, Salem, The Dalles, and West Linn.
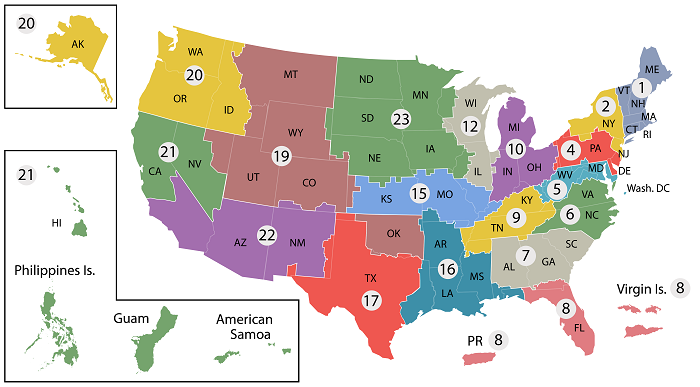
- VISN 1: VA New England Healthcare System
- VISN 2: New York/New Jersey VA Health Care Network
- VISN 4: VA Healthcare - VISN 4
- VISN 5: VA Capitol Health Care Network
- VISN 6: VA Mid-Atlantic Health Care Network
- VISN 7: VA Southeast Network
- VISN 8: VA Sunshine Healthcare Network
- VISN 9: VA MidSouth Healthcare Network
- VISN 10: VA Healthcare System
- VISN 12: VA Great Lakes Health Care System
- VISN 15: VA Heartland Network
- VISN 16: South Central VA Health Care Network
- VISN 17: VA Heart of Texas Health Care Network
- VISN 19: Rocky Mountain Network
- VISN 20: Northwest Network
- VISN 21: Sierra Pacific Network
- VISN 22: Desert Pacific Healthcare Network
- VISN 23: VA Midwest Health Care Network



















